Large study provides scientists with deeper insight into long COVID symptoms
Thursday, May 25, 2023
Large study provides scientists with deeper insight into long COVID symptoms
Initial findings from a study of nearly 10,000 Americans, many of whom had COVID-19, have uncovered new details about long COVID, the post-infection set of conditions that can affect nearly every tissue and organ in the body. Clinical symptoms can vary and include fatigue, brain fog, and dizziness, and last for months or years after a person has COVID-19. The research team, funded by the National Institutes of Health, also found that long COVID was more common and severe in study participants infected before the 2021 Omicron variant.
The study, published in JAMA, is coordinated through the NIH’s Researching COVID to Enhance Recovery (RECOVER) initiative, a nationwide effort dedicated to understanding why some people develop long-term symptoms following COVID-19, and most importantly, how to detect, treat, and prevent long COVID. The researchers hope this study is the next step toward potential treatments for long COVID, which affects the health and wellbeing of millions of Americans.
“Americans living with long COVID want to understand what is happening with their bodies,” said ADM Rachel L. Levine, M.D., Assistant Secretary for Health. “RECOVER, as part of a broader government response, in collaboration with academia, industry, public health institutions, advocacy organizations and patients, is making great strides toward improving our understanding of long COVID and its associated conditions.”
Researchers examined data from 9,764 adults, including 8,646 who had COVID-19 and 1,118 who did not have COVID-19. They assessed more than 30 symptoms across multiple body areas and organs and applied statistical analyses that identified 12 symptoms that most set apart those with and without long COVID: post-exertional malaise, fatigue, brain fog, dizziness, gastrointestinal symptoms, heart palpitations, issues with sexual desire or capacity, loss of smell or taste, thirst, chronic cough, chest pain, and abnormal movements.
They then established a scoring system based on patient-reported symptoms. By assigning points to each of the 12 symptoms, the team gave each patient a score based on symptom combinations. With these scores in hand, researchers identified a meaningful threshold for identifying participants with long COVID. They also found that certain symptoms occurred together and defined four subgroups or “clusters” with a range of impacts on health.
Based on a subset of 2,231 patients in this analysis who had a first COVID-19 infection on or after Dec. 1, 2021, when the Omicron variant was circulating, about 10% experienced long-term symptoms or long COVID after six months. The results are based on a survey of a highly diverse set of patients and are not final. Survey results will next be compared for accuracy against an array of lab tests and imaging.
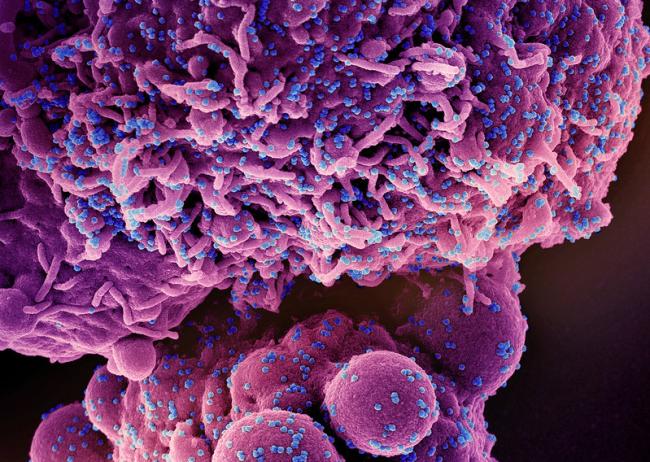
To date, more than 100 million Americans have been infected with SARS-CoV-2, the virus that causes COVID-19. As of April, the federal government’s Household Pulse survey estimates that about 10% of adults infected with the virus continue to experience and suffer from the many symptoms termed together as long COVID. Patients and researchers have identified more than 200 symptoms associated with long COVID.
“This study is an important step toward defining long COVID beyond any one individual symptom,” said study author Leora Horwitz, M.D., director of the Center for Healthcare Innovation and Delivery Science, and co-principal investigator for the RECOVER Clinical Science Core, at NYU Langone Health. “This approach — which may evolve over time — will serve as a foundation for scientific discovery and treatment design.”
The researchers explain studying the underlying biological mechanisms of long COVID is central to advancing informed interventions and identifying effective treatment strategies.
In addition to establishing the scoring system, the researchers found that participants who were unvaccinated or who had COVID-19 before the Omicron strain emerged in 2021 were more likely to have long COVID and more severe cases of long COVID. Further, reinfections were also linked to higher long COVID frequency and severity, compared to people who only had COVID-19 once.
“While the score developed in this study is an important research tool and early step toward diagnosing and monitoring patients with long COVID, we recognize its limitations,” said David C. Goff, M.D., Ph.D., director of the Division of Cardiovascular Sciences at the National Heart, Lung, and Blood Institute, part of NIH. Goff serves as an epidemiology lead for NIH RECOVER. “All patients suffering from long COVID deserve the attention and respect of the medical field, as well as care and treatment driven by their experiences. As treatments are developed, it will be important to consider the complete symptom profile.”
The ongoing RECOVER research serves as the foundation for planned clinical trials, whose interventions are rooted in many of the symptoms outlined in this study. RECOVER clinical trials are expected to begin enrolling patient participants in 2023.
This research was funded by NIH agreements OT2HL161841, OT2HL161847, and OT2HL156812. Additional support came from grant R01 HL162373. For more information on RECOVER, visit https://recovercovid.org.
About RECOVER: The National Institutes of Health Researching COVID to Enhance Recovery (NIH RECOVER) Initiative is a $1.15 billion effort, including support through the American Rescue Plan Act of 2021, that seeks to identify how people recuperate from COVID-19, and who are at risk for developing post-acute sequelae of SARS-CoV-2 (PASC). Researchers are also working with patients, clinicians, and communities across the United States to identify strategies to prevent and treat the long-term effects of COVID – including long COVID. For more information, please visit recovercovid.org.
HHS Long COVID Coordination: This work is a part of the National Research Action Plan (opens pdf), a broader government-wide effort in response to the Presidential Memorandum directing the Secretary for the Department of Health and Human Services to mount a full and effective response to long COVID. Led by Assistant Secretary for Health Admiral Rachel Levine, the Plan and its companion Services and Supports for Longer-term Impacts of COVID-19 (opens pdf) report lay the groundwork to advance progress in the prevention, diagnosis, treatment, and provision of services for individuals experiencing long COVID.
About the National Institutes of Health (NIH): NIH, the nation's medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit www.nih.gov.
NIH…Turning Discovery Into Health®
On May 31, 2023, a statistic in the seventh paragraph on the percentage of adults continuing to experience symptoms of COVID-19 was updated from 6% to 10%.
Institute/Center
Contact
301-496-5449


