NIH-funded team develops method to identify future SARS-CoV-2 mutations that could affect rapid antigen test performance
Thursday, September 15, 2022
NIH-funded team develops method to identify future SARS-CoV-2 mutations that could affect rapid antigen test performance
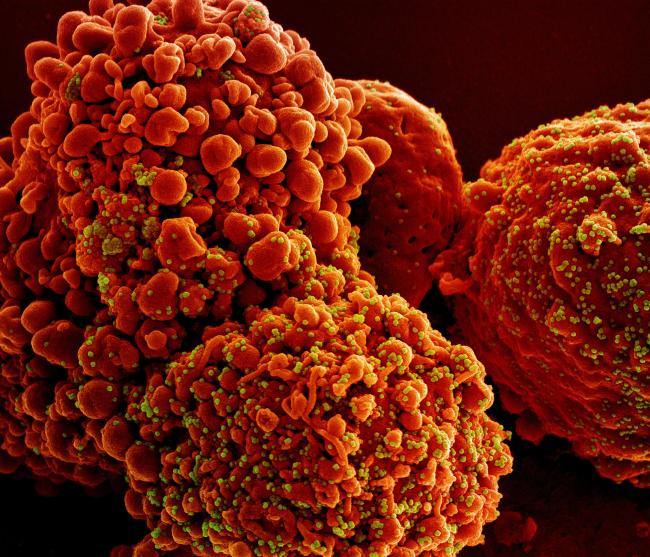
A research team funded by the National Institutes of Health has shown that commercially available rapid antigen tests can detect past and present variants of concern and has identified potential mutations that may impact test performance in the future. As new variants of the SARS-CoV-2 virus continue to emerge, concerns have been raised about the performance of rapid antigen tests.
The team, which was funded by NIH’s Rapid Acceleration of Diagnostics (RADx®) Tech program, developed a method to evaluate how mutations to SARS-CoV-2 can affect recognition by antibodies used in rapid antigen tests. Since most rapid antigen tests detect the SARS-CoV-2 nucleocapsid protein, or N protein, the team directly measured how mutations to the N protein impacted diagnostic antibodies’ ability to recognize their target.
“Rapid antigen tests remain an important COVID-19 mitigation tool, and it is essential to ensure that these tests can detect the SARS-CoV-2 virus as it continues to evolve,” said Bruce J. Tromberg, Ph.D., director of the National Institute of Biomedical Imaging and Bioengineering (NIBIB) and lead for the RADx Tech program at the NIH. “Considering the endless cycle of new variants, the data from this study will be useful for years to come.”
The study, published in Cell, used a method called deep mutational scanning to simultaneously evaluate how any single amino acid substitution in the N protein could affect diagnostic antibody binding. The researchers generated an exhaustive library of N protein variations, which includes nearly 8,000 single amino acid substitutions – representing more than 99.5% of all possible mutations – and evaluated their interaction with 17 different diagnostic antibodies used in 11 commercially available rapid antigen tests. Rapid antigen tests often employ two different diagnostic antibodies for the detection of the SARS-CoV-2 virus.
For each diagnostic antibody evaluated, the researchers documented which mutations to the N protein affected antibody recognition. From this information, they created an ‘escape mutation profile’ for each antibody, which lists the specific mutations to the N protein that have an effect on the antibody’s ability to bind to its target. While several diagnostic antibodies recognized the same region of the N protein, the researchers found that each antibody had a unique escape mutation profile. As the SARS-CoV-2 virus continues to develop mutations, this data can be used to flag specific antibodies whose diagnostic performance may need to be re-assessed.
“Based on our findings, none of the major past and present SARS-CoV-2 variants of concern contain N protein mutations that would affect recognition by antibodies used in current rapid antigen tests,” said first study author Filipp Frank, Ph.D., an assistant professor in the department of biochemistry at Emory University, Atlanta. “Further, this data could inform test design by identifying which diagnostic antibodies should be paired to identify the maximum amount of potential N protein variations.”
“Accurate and efficient identification of infected individuals remains a critically important strategy for COVID-19 mitigation, and our study provides information about future SARS-CoV-2 mutations that may interfere with detection,” said senior study author Eric Ortlund, Ph.D., a professor in the department of biochemistry at Emory University. “The results outlined here can allow us to quickly adapt to the virus as new variants continue to emerge, representing an immediate clinical and public health impact.”
While many variants of concern contain multiple mutations to the N protein, the study authors note that their method does not evaluate how multiple mutations could affect diagnostic antibody recognition, representing a limitation of the study.
The project was supported in part by funds from the American Rescue Plan Act of 2021 administered by NIBIB under award numbers U54EB015408 and U54EB027690. The work was also supported under award number 75N92019P00328. This support was part of the RADx initiative, launched to speed innovation in the development, commercialization, and implementation of technologies for COVID-19 testing.
Researchers were also supported by the National Institute of Diabetes and Digestive and Kidney Diseases under award number R01DK115213; the National Institute of Allergy and Infectious Diseases under award number K99AI153736; and the American Heart Association under career development award 848388.
About the Rapid Acceleration of Diagnostics (RADx®) initiative: The RADx initiative was launched on April 29, 2020, to speed innovation in the development, commercialization, and implementation of technologies for COVID-19 testing. The initiative has four programs: RADx Tech, RADx Advanced Technology Platforms, RADx Underserved Populations and RADx Radical. It leverages the existing NIH Point-of-Care Technology Research Network. The RADx initiative partners with federal agencies, including the Office of the Assistant Secretary of Health, Department of Defense, the Biomedical Advanced Research and Development Authority, and U.S. Food and Drug Administration. Learn more about the RADx initiative and its programs: https://www.nih.gov/radx.
About the National Institute of Biomedical Imaging and Bioengineering (NIBIB): NIBIB’s mission is to improve health by leading the development and accelerating the application of biomedical technologies. The Institute is committed to integrating the physical and engineering sciences with the life sciences to advance basic research and medical care. NIBIB supports emerging technology research and development within its internal laboratories and through grants, collaborations, and training. More information is available at the NIBIB website: https://www.nibib.nih.gov.
About the National Institutes of Health (NIH): NIH, the nation's medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit www.nih.gov.
NIH…Turning Discovery Into Health®
Filipp Frank, Meredith M. Keen, Anuradha Rao, Leda Bassit, Xu Liu, Heather B. Bowers, Anamika B. Patel, Michael L. Cato, Julie A. Sullivan, Morgan Greenleaf, Anne Piantadosi, Wilbur A. Lam, William H. Hudson, Eric A. Ortlund. Deep mutational scanning identifies SARS-CoV-2 Nucleocapsid escape mutations of currently available rapid antigen tests. Cell 2022. https://doi.org/10.1016/j.cell.2022.08.010.
Institute/Center
Contact
301-496-3500


