Phantom limb study rewires our understanding of the brain
Thursday, August 21, 2025
Phantom limb study rewires our understanding of the brain
NIH scientists and collaborators reveal the brain preserves its representation of lost limb in clinical study.
In a first-of-its-kind study, researchers found that the brain’s control center for a lost appendage can persist long after surgical amputation, which stands in stark contrast to longstanding theories about the brain’s ability to reorganize itself, also known as plasticity. Scientists from the National Institutes of Health (NIH) and their colleagues examined human brain activity before and after arm amputation and found that the loss of a limb does not prompt a large-scale cerebral overhaul. Published in the journal Nature Neuroscience, this study offers new insight into the mysterious phantom limb syndrome and could help guide the development of neuroprosthetics and pain treatments for people with limb loss.
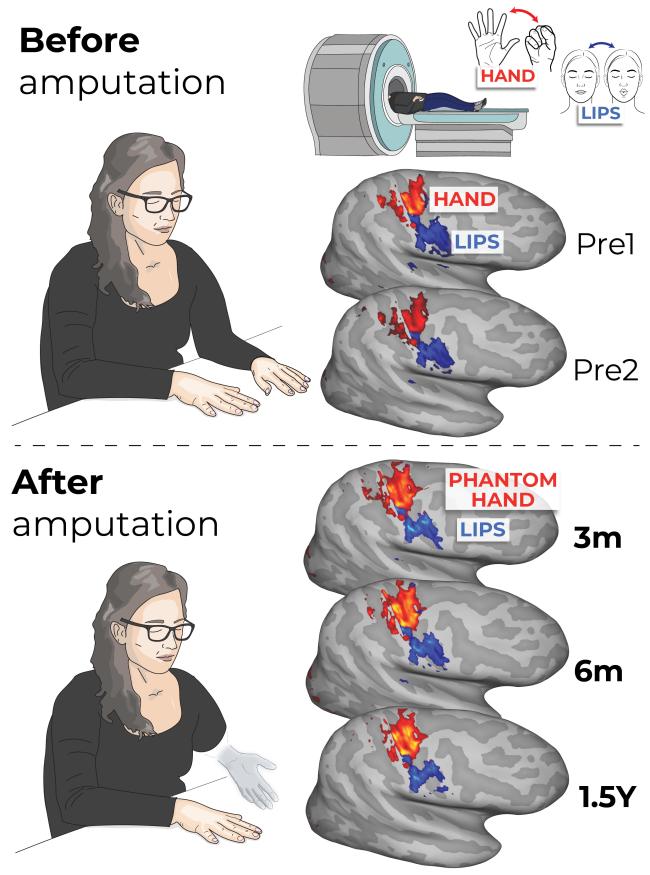
A team of scientists from NIH and University College London acted on a unique window of opportunity, running MRI scans on three participants in the months prior to a planned amputation (performed for separate medical purposes) and then up to five years after.
“It’s not often you get the chance to conduct a study like this one, so we wanted to be exceedingly thorough,” said co-author Chris Baker, Ph.D., of NIH’s National Institute of Mental Health (NIMH). “We approached our data from a variety of angles and all of our results tell a consistent story.”
Different regions in the brain’s outermost layer, called the cortex, are responsible for managing specific body parts. A prevailing theory among neuroscientists has been that, when a body part is damaged or lost, the cortex will remap itself, with neighboring regions associated with intact body parts encroaching on the newly available real estate.
“For many decades, cortical remapping as a response to amputation has been a literal textbook example of brain plasticity,” Baker said.
This corner of neuroscience has not been without debate, however. One sticking point with this theory is the pervasive phantom limb syndrome, wherein a patient feels vivid, often painful, sensations in a now missing extremity.
Baker and his co-authors took this phenomenon as a hint that the brain may remember what it lost. To find out for sure, the researchers needed to do something unprecedented; compare individuals’ brain activity before and after their amputation.
After many years of actively searching for and screening patients that were already scheduled to undergo amputation, the researchers identified three participants who could help answer their questions.
Twice before the planned arm amputations, the scientists scanned participants using a special type of MRI, called functional MRI, to map brain activity triggered by the tapping of individual fingers. In the months and years following the surgeries, the researchers conducted three follow-up scans on the participants as they attempted to perform the same tasks, now with their phantom limb.
The researchers then compared brain activity in search of any major changes between pre- and post-amputation data, but it quickly became clear that there was little to no difference. Had the authors not already known when the data was collected, Baker explained, then they likely would not have been able to tell the difference between the brain maps.
The team’s analysis was not limited to human eyes, however. The authors found that a machine learning algorithm — trained to identify movements of the fingers from pre-amputation data —had no trouble distinguishing which phantom finger was being moved after amputation.
The researchers also learned that nearby brain circuits associated with lip and feet movement did not migrate into the phantom limb’s territory. Additional analyses comparing their data to scans of able-bodied controls, as well as to other studies entirely, only continued to bolster their initial impression; the brain’s representation of the lost limb endures.
These results potentially improve our understanding of how phantom limb syndrome manifests and suggest that standard phantom pain treatments — many of which assume cortical reorganization after limb loss — may be worth rethinking. According to the study’s lead author, Hunter Schone, Ph.D., who conducted this research while a graduate student at NIH, the findings could also be key in how we implement transformative brain-computer interface technologies.
"This study is a powerful reminder that even after limb loss, the brain holds onto the body, almost like it’s waiting to reconnect in some new way,” said Schone. “Now, rapidly developing brain-computer interface technologies can operate under the assumption that the brain's body map remains consistent over time. This allows us to move into the next frontier: accessing finer details of the hand map, like distinguishing the tip of the finger from the base, and restoring the rich, qualitative aspects of sensation, such as texture, shape and temperature.”
About the National Institutes of Health (NIH): NIH, the nation's medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit www.nih.gov.
NIH…Turning Discovery Into Health®
Reference
'Stable cortical body maps before and after arm amputation.' Nature Neuroscience. 2025. DOI: 10.1038/s41593-025-02037-7
Institute/Center
Contact
301-496-5787


