Study suggests way to improve flu vaccines
April 17, 2018
Study suggests way to improve flu vaccines
At a Glance
- Researchers found that, while flu virus infections induce a strong immune response to the virus surface protein neuraminidase, seasonal flu vaccines do not.
- Current vaccines mainly target hemagglutinin, a more abundant flu surface protein.
- The study suggests that vaccines designed to target neuraminidase could offer broader protection against different virus strains and lessen severity of illness.
Influenza, or flu, is caused by a group of related viruses that infect the nose, throat, and lungs. Each year, thousands of people nationwide die from flu and its complications. Seasonal flu vaccines are the most effective way to protect against the disease. However, the vaccine does not prevent all flu illnesses.
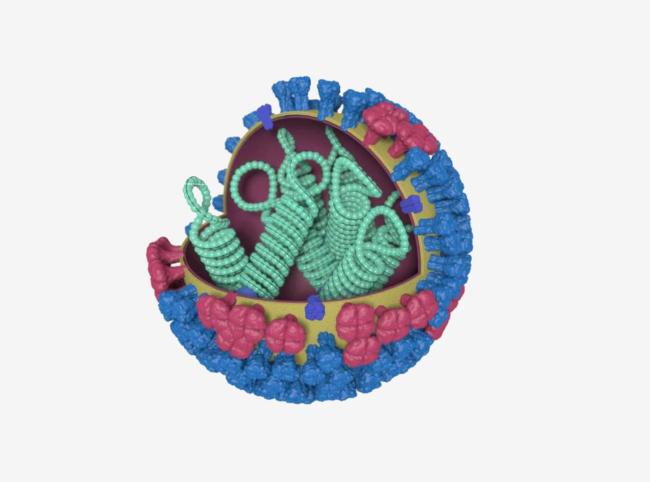
Flu viruses have two main types of surface proteins: hemagglutinin (HA) and neuraminidase (NA). Seasonal flu vaccines are developed and evaluated based mostly on their ability to prompt the immune system to make antibodies against HA, the more abundant surface protein. Previous research, however, found that anti-NA antibodies may be more important than anti-HA antibodies for protecting people from severe flu symptoms.
A research team led by Dr. Patrick Wilson at the University of Chicago Medicine and Dr. Florian Krammer at the Icahn School of Medicine at Mt. Sinai set out to examine human antibody responses to NA. Their work was funded by NIH’s National Institute of Allergy and Infectious Diseases (NIAID), through its Centers of Excellence for Influenza Research and Surveillance program, and the Food and Drug Administration. Results were published on April 5, 2018, in Cell.
The team examined blood samples from people who were vaccinated against flu and those who were diagnosed with either the H3N2 or H1N1 influenza viruses. They found that flu vaccines rarely induced anti-NA antibodies. In contrast, natural flu infection induced anti-NA antibodies at least as often as anti-HA ones.
Lab experiments showed that anti-NA antibodies induced during natural flu infection reacted against diverse strains of flu virus. To test whether they could also protect against diverse strains, the researchers isolated anti-NA antibodies from the H3N2 and H1N1 influenza patients. When the team gave anti-NA antibodies derived from the H3N2 patients to mice and infected the mice with a different H3N2 virus strain, 11 of the 13 tested antibodies protected the mice. Four of eight anti-NA antibodies derived from the H1N1 patients protected mice against both a similar H1N1 virus strain and an H5N1-like strain. Past studies have found far less overlap among anti-HA antibodies.
These findings suggest that flu vaccines designed to target NA may provide broader protection against diverse virus strains. To this end, scientists continue to study immune system responses to NA.
“Our results demonstrate that hemagglutinin should no longer be the de facto target in influenza vaccine development efforts,” Wilson says. “We think including an improved neuraminidase component to future influenza vaccine compositions can reduce the severity of illness and decrease the frequency of community-acquired influenza infections.”
Related Links
- Finding Factors That Protect Against Flu
- Microneedle Patch for Flu Vaccine
- Strategy May Improve Seasonal Flu Vaccines
- Safeguarding Our Health: Vaccines Protect Us All
- Influenza
- Centers of Excellence for Influenza Research and Surveillance (CEIRS)


