Cancer cells drain energy from immune cells
December 7, 2021
Cancer cells drain energy from immune cells
At a Glance
- Researchers found that cancer cells use straw-like nanotubes to siphon mitochondria from immune cells, essentially draining their energy.
- Inhibiting nanotube formation could make certain anticancer therapies more effective.
Cancer cells must evade the immune system to grow and spread. One way they do so is by presenting proteins on their surfaces that dampen the ability of immune cells to kill them. A type of cancer therapy called immune checkpoint inhibition blocks the interaction of these proteins with immune cells. This allows the immune cells to more efficiently kill the cancer. But this treatment doesn’t work in all cases, suggesting that cancer cells have other tricks up their sleeve for evading the immune system.
A team of researchers led by Drs. Hae Lin Jang and Shiladitya Sengupta at Brigham and Women’s Hospital investigated how cancer cells escape the immune system by growing human and mouse breast cancer cells with T cells, a type of immune cell. NIH’s National Cancer Institute (NCI) and National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) supported the research. The findings appeared in Nature Nanotechnology on November 18, 2021.
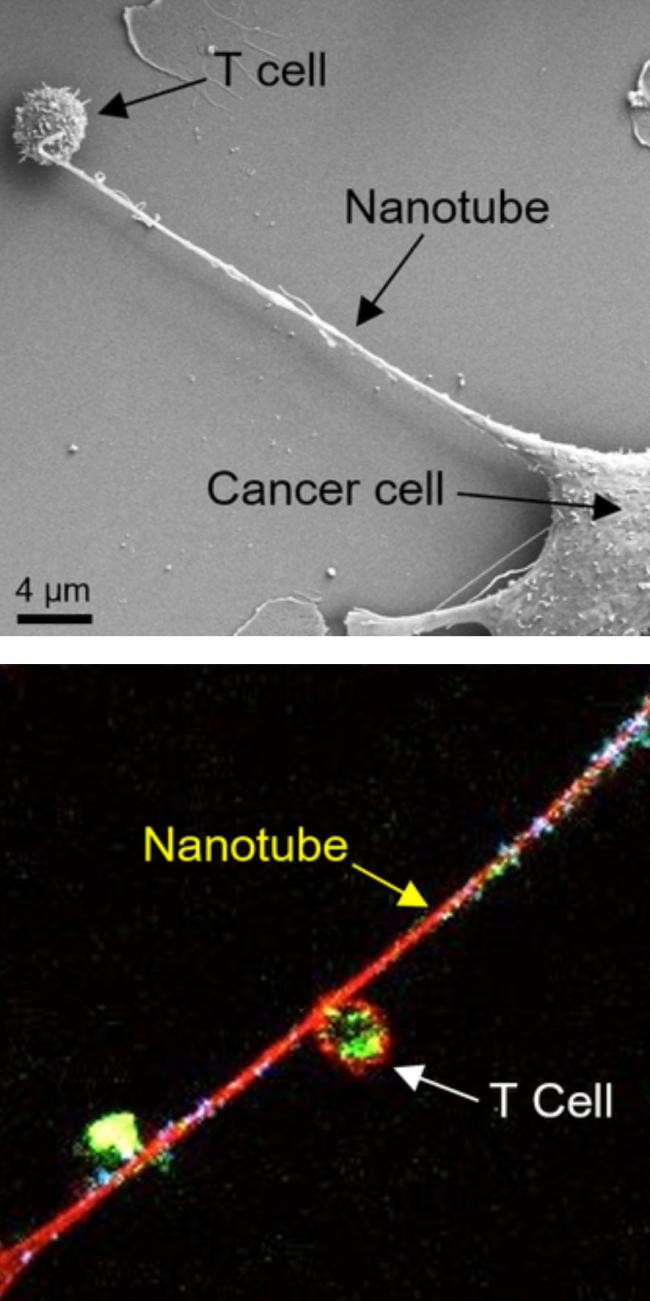
Under an electron microscope, the researchers saw long, hollow appendages called nanotubes connecting the cancer cells and T cells. Previous research has found similar structures being used to transfer material between cells.
Next, they stained mitochondria, which generate energy for cells, in the T cells with a fluorescent dye. Sixteen hours after adding these stained cells to a cancer cell culture, they saw fluorescent mitochondria from the immune cells moving through the nanotubes and into the cancer cells. Of note, this transfer was largely one-way; mitochondria didn’t go from the cancer cells to the T cells.
The transfer of mitochondria affected the metabolism of both cell types. Cancer cells consumed oxygen at a faster rate when grown together with T cells. This indicated that mitochondria in the cancer cells were producing more energy. The cancer cells also grew more in the presence of the T cells. Meanwhile, the T cell population declined rapidly.
The team tried inhibiting the machinery that cells use to construct nanotubes by various means. In each case, doing so reduced mitochondrial transfer to cancer cells. This suggested that targeting nanotube formation could be therapeutic. The researchers tested this idea in a mouse model of breast cancer. They treated the mice with a combination of an inhibitor of nanotube formation and an immune checkpoint inhibitor. Doing so reduced tumor growth more than either drug alone.
These results suggest that cancer cells siphon mitochondria from T cells. This helps energize the cancer cells and, at the same time, disable the immune cells. Inhibiting nanotube formation could thus increase the efficacy of immune checkpoint inhibitor therapies for cancer. The authors point out that the nanotube inhibitors they tested have other effects. Compounds that specifically target nanotube formation will need to be developed before the treatment could be tried in patients.
“Cancer kills when the immune system is suppressed and cancer cells are able to metastasize, and it appears that nanotubes can help them do both,” Sengupta says. “This is a completely new mechanism by which cancer cells evade the immune system, and it gives us a new target to go after.”
—by Brian Doctrow, Ph.D.
Related Links
- Predicting Response to Immunotherapy
- Breast Cancer Patient Benefits from Modified Immunotherapy
- Personalized Immunotherapy Treats Epithelial Cancer
- Exosomes May Help Tumors Evade Immune System
- Immunotherapy to Treat Cancer
- Immune Checkpoint Inhibitors
References
Intercellular nanotubes mediate mitochondrial trafficking between cancer and immune cells. Saha T, Dash C, Jayabalan R, Khiste S, Kulkarni A, Kurmi K, Mondal J, Majumder PK, Bardia A, Jang HL, Sengupta S. Nat Nanotechnol. 2021 Nov 18. doi: 10.1038/s41565-021-01000-4. Online ahead of print. PMID: 34795441.
Funding
NIH’s National Cancer Institute (NCI) and National Institute of Arthritis Musculoskeletal and Skin Diseases (NIAMS); American Lung Association; United States Department of Defense.


