Nanoparticles developed for traumatic brain injury
January 12, 2021
Nanoparticles developed for traumatic brain injury
At a Glance
- Researchers designed a system to effectively deliver drugs across the blood brain barrier in mice using nanoparticles.
- The delivery system could be used to treat a variety of neurological disorders.
A bump, blow, or jolt to the head can cause a traumatic brain injury (TBI). More than 2 million people in the U.S. sustain TBIs each year. Falls, car accidents, and sports injuries are among common causes. A severe TBI can result in long-lasting problems with brain function, memory, and speech. TBIs may also increase the likelihood of developing diseases like Alzheimer’s and Parkinson’s disease, which cause brain cells to degenerate.
TBI treatments are limited and focus mainly on preventing further brain damage. Drugs that might help prevent Alzheimer’s and other neurodegenerative diseases after TBI are hard to deliver to brain tissue. They’re hampered by a dense barrier of cells protecting the brain called the blood brain barrier. This barrier prevents harmful materials that circulate in the blood from entering the brain, while allowing in oxygen, water, and other vital substances. As a result, doctors only have the short, unpredictable period when the blood brain barrier is breached after a head injury to deliver drugs to brain tissue.
A research team led by Drs. Rebekah Mannix, Jeffrey Karp, and Nitin Joshi set out to develop a system that would allow therapeutics to cross the blood brain barrier while intact. The team, centered at Brigham and Women's Hospital, Harvard Medical School, and Boston Children's Hospital, was funded in part by NIH’s National Heart, Lung, and Blood Institute (NHLBI). Findings were published in Science Advances on January 1, 2021.
The team engineered nanoparticles to carry a promising TBI drug to the brain. The drug was a small interfering RNA (siRNA) molecule designed to inhibit the production of tau protein. siRNA molecules are a new class of therapeutics that can be used for the targeted silencing of genes, essentially turning them off. Tau is thought to play a key role in Alzheimer’s and related diseases.
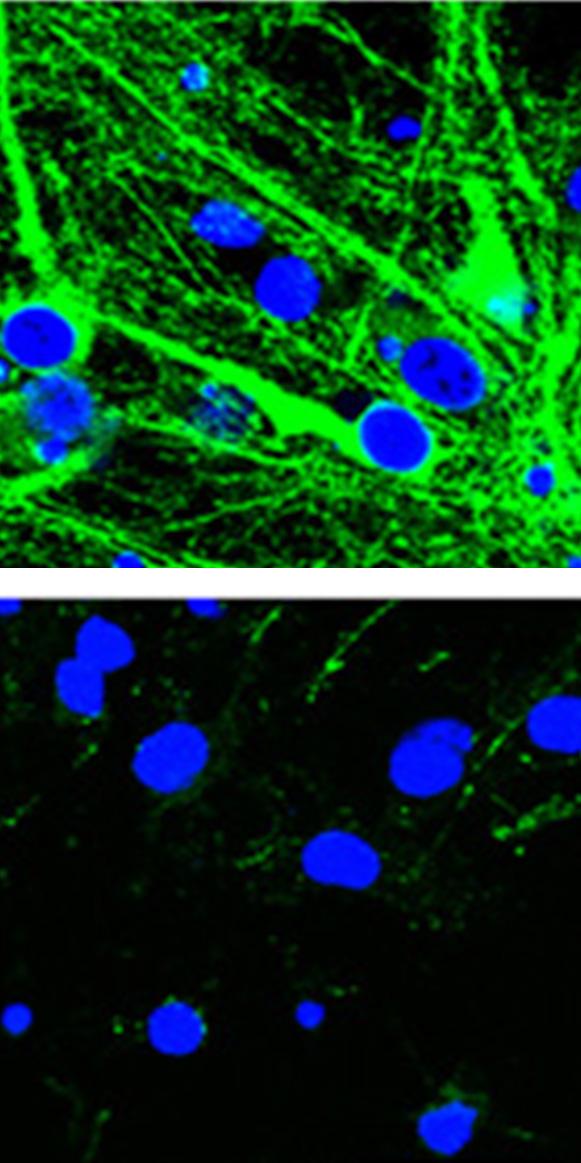
The scientists formulated the nanoparticles using PGLA, a polymer used in several FDA-approved products. They experimented with different surface coatings to find a nanoparticle design that could most effectively penetrate the blood brain barrier. They carried out studies in healthy mice to identify the most effective at delivering drugs to the brain.
Using a mouse model of TBI, they then showed that the optimized nanoparticles, which were coated with defined amounts of a compound called Polysorbate 80, could reach the brain both before and after the blood brain barrier was repaired. IV injections of the engineered nanoparticles resulted in threefold higher brain accumulation of siRNA compared to nanoparticles that had not been optimized.
Finally, the researchers found that mice with TBI who received the optimized siRNA nanoparticles had a 50% reduction in tau. This was true even when the nanoparticles were given late in an injury, outside the window that the blood brain barrier was breached. No reduction in tau was seen in mice given siRNA using a conventional delivery system.
These findings suggest that the nanoparticle platform holds promise for treating TBI as well as other neurological disorders.
“The technology developed for this publication could allow for the delivery of a large number of diverse drugs, including antibiotics, antineoplastic agents, and neuropeptides,” Mannix says. “This could be a game changer for many diseases that manifest in the central nervous system.”
—by Erin Bryant
Related Links
- Biomarkers Predict Concussion Recovery Time
- Blood Proteins Associated with Persistent Symptoms After Brain Injury
- Tiny Bleeds Associated With Disability After Brain Injury
- Many With Mild Traumatic Brain Injury Don’t Receive Follow-up Care
- Predicting Recovery Time for Sports Concussions
- Insights into Brain Injury
- Caring for Concussions
- Traumatic Brain Injury Information Page
References
BBB pathophysiology–independent delivery of siRNA in traumatic brain injury. Wen Li, Jianhua Qiu, Xiang-Ling Li, Sezin Aday, Jingdong Zhang, Grace Conley, Jun Xu, John Joseph, Haoyue Lan, Robert Langer, Rebekah Mannix, Jeffrey M. Karp, Nitin Joshi. Science Advances. 01 Jan 2021: Vol. 7, no. 1, eabd6889. DOI: 10.1126/sciadv.abd6889.
Funding
NIH’s National Heart, Lung, and Blood Institute (NHLBI); Fundação para a Ciência e a Tecnologia; National Football League Players Association.


