Unexpected role for the nervous system in anaphylaxis
April 4, 2023
Unexpected role for the nervous system in anaphylaxis
At a Glance
- Researchers found evidence that the nervous system plays a key role in the extreme and sometimes deadly allergic reactions known as anaphylaxis.
- The findings from this mouse study may point to new approaches for treating or even preventing anaphylaxis in humans.
Anaphylaxis is a life-threatening allergic reaction that can be triggered by certain foods, medications, or insect bites. The immune system releases a flood of chemicals that can cause people to go into shock—a dangerous drop in blood pressure that deprives the body of oxygen. Standard treatment is an injection of epinephrine, which can quickly restore blood pressure. It does this in part by rapidly constricting blood vessels. There are no effective ways to prevent anaphylaxis and shock, besides avoiding the triggering substances, called allergens.
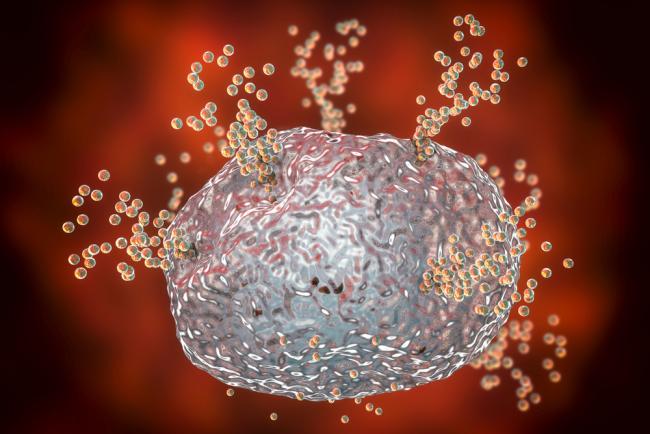
Immune cells called mast cells are known to play a key role in anaphylaxis. These cells are found near blood vessels and nerves in various tissues throughout the body. When exposed to certain allergens in blood, mast cells can provoke a body-wide response. They release histamines and other substances that are believed to prompt dilation and leakage of blood vessels. That leads to the rapid blood pressure drop typical of anaphylactic shock in humans. In some animals, anaphylaxis is also marked by a sudden drop in core body temperature. This drop might play a harmful role in anaphylaxis in people as well.
A research team led by Dr. Soman N. Abraham of Duke University Medical Center examined the mechanisms that underlie the rapid drop in body temperature seen in mice with anaphylaxis. Earlier studies had hinted that a neural circuit that helps to regulate body temperature might play a role. But to date, only the immune system—and not the nervous system—had been implicated in anaphylaxis. The findings were published online in Science Immunology on March 17, 2023.
In a series of experiments, the researchers found evidence that during anaphylaxis, heat-sensing nerve cells in mice became highly activated, despite the fact that no heat was being applied. This created a false signal that the body was overheating.
Further study revealed that during anaphylaxis, mast cells release an enzyme called chymase, which interacts with a protein called TRPV1 on a subset of sensory nerve cells. This interaction triggers a sudden shutdown of heat-generating brown fat cells. The result was a rapid drop in body temperature characteristic of anaphylaxis.
To validate these findings, the scientists showed that mice lacking chymase or TRPV1 were protected against a sudden drop in body temperature during anaphylaxis. Direct activation of TRPV1 nerve cells led to a rapid drop in body temperature even without exposure to allergens.
“By demonstrating that the nervous system is a key player—not just the immune cells—we now have potential targets for prevention or therapy,” says first author Chunjing “Evangeline” Bao. “This finding could also be important for other conditions, including septic shock, and we are undertaking those studies.”
—by Vicki Contie
Related Links
- Uncovering the Origins of Brown Fat
- How Brown Fat Improves Metabolism
- Unexplained Cases of Anaphylaxis Linked to Red Meat Allergy
- Researchers Link Protein to Drug Allergies
- Sensing Temperature
- Drug Allergies: What to Look Out For
- Understanding Food Allergies: How to Prevent Peanut Allergy and More
- Anaphylaxis
References
A mast cell-thermoregulatory neuron circuit axis regulates hypothermia in anaphylaxis. Bao C, Chen O, Sheng H, Zhang J, Luo Y, Hayes BW, Liang H, Liedtke W, Ji RR, Abraham SN. Sci Immunol. 2023 Mar 17;8(81): eadc9417. doi: 10.1126/sciimmunol.adc9417. Epub 2023 Mar 17. PMID: 36930731.
Funding
NIH’s National Institute of General Medical Sciences (NIGMS).


