Genetic variant associated with absence of COVID-19 symptoms
August 8, 2023
Genetic variant associated with absence of COVID-19 symptoms
At a Glance
- Researchers identified a genetic variant found in many people who didn’t develop symptoms when they were infected by SARS-CoV-2.
- Understanding how this variant helped people fend off the virus could lead to better ways to protect against COVID-19.
At least 20% of people infected with SARS-CoV-2, the virus that causes COVID-19, never showed symptoms. These asymptomatic infections could provide clues to how the virus can be quickly cleared from the body. Genetic factors may be involved. However, most studies of genetics and COVID-19 outcomes to date have focused on severe disease.
An NIH-funded study looked for genetic variation associated with asymptomatic SARS-CoV-2 infections. The researchers examined how these variations affected the function of T cells, a part of the immune system that is key for fighting viral infections. Results appeared in Nature on July 19, 2023.
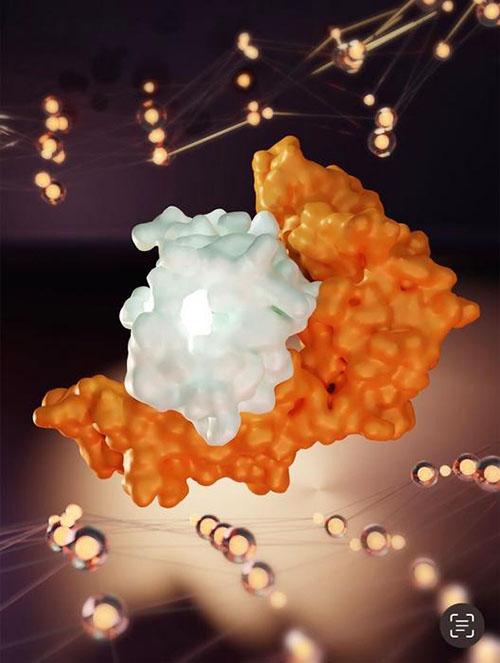
The team focused on a group of genes called the human leukocyte antigen (HLA) complex. The proteins encoded by these genes help the immune system to recognize infected or foreign cells by displaying pieces of pathogens for T cells to identify. HLA genes vary greatly among people.
To find HLA variants associated with asymptomatic COVID-19, the researchers recruited nearly 30,000 bone marrow donors. Since HLA genes determine the compatibility of tissue or organ donors and recipients, these people already had their HLA genes sequenced. Study participants used a smartphone app to track COVID-19 symptoms and report positive tests for SARS-CoV-2. Nearly 1,500 of participants who were unvaccinated reported a positive test.
Analysis of HLA genes among this group revealed that one variant, called HLA-B*15:01, was more common in asymptomatic participants (20%) than in symptomatic ones (9%). The effect was confirmed in two other groups of people.
The team next examined how HLA-B*15:01 affected the ability of T cells to recognize SARS-CoV-2. They studied T cells from people with HLA-B*15:01 that had been donated before the COVID-19 pandemic. These T cells, they found, reacted to a particular piece of SARS-CoV-2 as though they had encountered it before. Further experiments showed that T cells recognizing this SARS-CoV-2 fragment also recognized a similar fragment from coronaviruses that cause seasonal colds. Both fragments bound to the HLA-B*15:01 protein in a similar manner. This shows that T cells that encountered and learned to recognize seasonal coronaviruses could also recognize SARS-CoV-2.
The findings suggest that T cells in many people with HLA-B*15:01 could already recognize SARS-CoV-2 because of their prior exposure to seasonal coronaviruses. This allowed their immune systems to respond quickly and clear out the virus before it could cause any symptoms.
“If you have an army that’s able to recognize the enemy early, that’s a huge advantage,” says study coauthor Dr. Jill Hollenbach of the University of California, San Francisco. “It’s like having soldiers that are prepared for battle and already know what to look for, and that these are the bad guys.”
These results could help guide the development of better vaccines or drugs for preventing and treating COVID-19.
—by Brian Doctrow, Ph.D.
Related Links
- T Cells Protect Against COVID-19 in Absence of Antibody Response
- Antibodies and T Cells Protect Against SARS-CoV-2
- Immune Cells for Common Cold May Recognize SARS-CoV-2
- COVID-19 Research
- COVID-19 Prevention Network
- Immune System Research
- COVID-19 (CDC)
References
A common allele of HLA is associated with asymptomatic SARS-CoV-2 infection. Augusto DG, Murdolo LD, Chatzileontiadou DSM, Sabatino JJ Jr, Yusufali T, Peyser ND, Butcher X, Kizer K, Guthrie K, Murray VW, Pae V, Sarvadhavabhatla S, Beltran F, Gill GS, Lynch KL, Yun C, Maguire CT, Peluso MJ, Hoh R, Henrich TJ, Deeks SG, Davidson M, Lu S, Goldberg SA, Kelly JD, Martin JN, Vierra-Green CA, Spellman SR, Langton DJ, Dewar-Oldis MJ, Smith C, Barnard PJ, Lee S, Marcus GM, Olgin JE, Pletcher MJ, Maiers M, Gras S, Hollenbach JA. Nature. 2023 Jul 19. doi: 10.1038/s41586-023-06331-x. Online ahead of print. PMID: 37468623.
Funding
NIH’s National Institute of Allergy and Infectious Diseases (NIAID), National Institute of Biomedical Imaging and Bioengineering (NIBIB), National Human Genome Research Institute (NHGRI), National Cancer Institute (NCI), and National Heart, Lung, and Blood Institute (NHLBI); National Health and Medical Research Council; Medical Research Future Fund; Health Resources and Services Administration; Office of Naval Research; Be the Match Foundation; Medical College of Wisconsin; National Marrow Donor Program.


