You are here
Brain and Mental Health
Couples Therapy
Based on over 30 years of research funded by the NIH, the Prevention and Relationship Enhancement Program is the most widely used, empirically based approach to helping couples build emotional safety and effectively manage issues and conflict.
Image credit: Daniel Soñé/NCI
- The Program works with couples to build and strengthen relationship skills, including communication and conflict management.
- Couples who complete the Program report up to 90% reductions in physical aggression through a 10-month follow-up compared to couples who received an alternative approach.
- Other outcomes of the Program include reductions in high-risk sexual behaviors, substance use, and weapon-carrying, and increases in relationship satisfaction and well-being.
Obsessive Compulsive Disorder
NIH-funded research led to the development of exposure and response prevention (ERP) treatment for obsessive-compulsive disorder (OCD), which was once thought to be untreatable. With improvement in symptoms in over half of patients, ERP is now the first treatment therapists turn to for OCD.
Image credit: National Institute on Aging, NIH
- OCD is a common, chronic, and long-lasting disorder in which a person has uncontrollable, reoccurring thoughts (obsessions) and/or behaviors (compulsions) that they feel the urge to repeat over and over.
- In ERP, people with OCD are gradually exposed to fear-provoking or discomforting stimuli related to their obsessions to help them practice resisting the urge to engage in compulsive behaviors.
- ERP can be used in parallel with medication and can also be helpful for people who do not respond to medication.
Phobias
Developed in part thanks to NIH research, exposure therapy is now considered the gold standard for treating phobias. For those who complete treatment, 80-90% report their fear significantly reduced or completely eliminated.
Image credit: National Institute on Aging, NIH
- Exposure therapy enables patients to overcome anxieties by gradually introducing them to feared scenarios or objects in a safe environment, often starting with small, indirect exposures, before progressing to more direct exposures.
- Behavior changes in response to a specific phobia is often maintained long-term, with 90% of patients still showing significant reduction in fear, avoidance, and overall level of impairment after 4 years, and 65% no longer having a specific phobia.
Depression
Through NIH-funded research and clinical trials, Cognitive Behavioral Therapy (CBT) is now the gold standard behavioral treatment for depression.
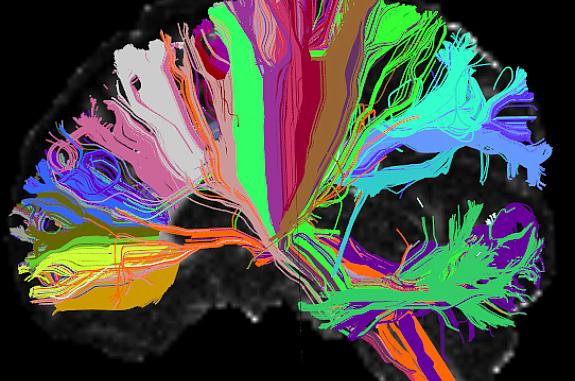
Image credit: Viviana Siless, Ph.D., Anastasia Yendiki, Ph.D., MGH/Harvard, Boston Adolescent Neuroimaging of Depression and Anxiety (BANDA)
- About 1 out of every 6 adults will have depression at some time in their life, and depression affects about 16 million American adults every year.
- NIH has funded over a thousand clinical trials on CBT and depression since the 1970s.
- CBT has been studied and adapted for children, adolescents, couples, and families.
- Other forms of CBT, such as Mindfulness-Based Cognitive Therapy, have also been developed and used to treat depression.
- Components of CBT have been found to be as effective as antidepressant medication in treating depression.
Psychosis
NIH-supported research led to more effective methods of treatment for early-stage psychosis and schizophrenia. More than 14,000 people per year in the U.S., are treated for schizophrenia using these best practices, and they experience substantially improved quality of life.
Image credit: Darryl Leja, National Human Genome Research Institute, NIH
- NIH research shows that early treatment of psychosis increases the chance of successful recovery.
- In addition to greater improvement in symptoms, quality of life, and work/school participation, this research also demonstrates that these treatment programs can be implemented in community-based settings.
- These best practices developed by NIH researchers are now the standard treatment for early psychosis, per the American Psychiatric Association’s Practice Guideline on Treatment of Patients with Schizophrenia.
Addiction Treatment
NIH-supported research on addiction has informed public health policies, such as the Mental Health Parity and Addiction Equity Act of 2008 (MPHAEA), which requires insurance providers to give the same coverage for substance use disorders and other mental illnesses as for other medical illnesses.
Image credit: Photo by Fortune Vieyra on Unsplash
- Decades of NIH-funded research has led to understanding addiction as a chronic, relapsing brain disorder.
- Rather than a moral weakness or a lack of willpower, we now know that addiction is characterized by changes in brain circuitry that interfere with the ability to exert self-control over substance use.
- NIH research has informed public health policies, such as MPHAEA, which are associated with increased enrollment and use of outpatient treatment services and reduced spending on emergency department visits and hospital stays among patients with substance use disorders.
Mood Stabilizers
NIH played a significant role in the development of the mood stabilizer lithium carbonate—one of the first medications used successfully to treat several psychiatric disorders—that continues to be used around the world today. Informed by NIH-supported research, current practice guidelines for bipolar disorder now include mood stabilizer medication as the first-line treatment.
Image credit: National Institute on Aging, NIH
- Mood stabilizers are typically used to treat bipolar disorder and mood changes associated with other mental disorders.
- In 1969, a seminal study at NIH showed the effectiveness of lithium carbonate treatment in depression and mania.
- Lithium is on the WHO’s List of Essential Medicines and continues to be used widely—especially in the treatment of bipolar disorder—impacting the lives of countless people around the world.
- The NIH Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) program showed the importance of mood stabilizer medication as the first-line treatment for bipolar disorder.
Deep Brain Stimulation
NIH made significant contributions to the development of deep brain stimulation (DBS), a treatment that can offer patients relief from symptoms in Parkinson’s disease and other brain disorders. By 2021, more than 200,000 DBS devices were estimated to have been implanted worldwide.
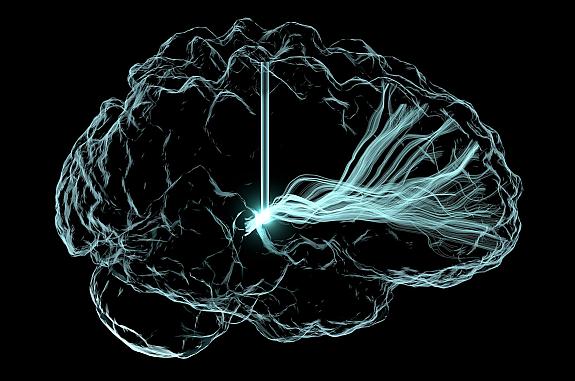
Image credit: Andrew Janson, Butson Lab, University of Utah
- NIH-supported research contributed to the development and clinical application of DBS, and a major clinical trial showed DBS for Parkinson’s disease was superior to L-DOPA, the current gold standard treatment alone.
- FDA approved the first DBS device for Parkinson’s disease in 2002, and devices are also approved or used experimentally for essential tremor, dystonia, epilepsy, Tourette syndrome, treatment-resistant depression, and chronic pain.
- In 2009, FDA approved DBS for treatment-resistant obsessive-compulsive disorder under a Humanitarian Device Exemption.
Dementia Biomarkers
Before the early 2000s, the only sure way to know whether a person had Alzheimer’s disease or another form of dementia was after death through autopsy. Thanks to NIH-supported research, tests are now available to help doctors measure biomarkers—biological indicators of disease—associated with dementia in a living person.
Image credit: Strittmatter Laboratory, Yale University
- Biomarkers are measurable indicators of what’s happening in the body, and can be found in blood, other body fluids, organs, and tissues.
- Biomarkers can be analyzed through brain imaging and genetic, cerebrospinal fluid, and blood testing.
- NIH supported the initial development of the PrecivityAD™ blood test, a commercially available tool for detecting biomarkers for beta-amyloid plaques, a hallmark of Alzheimer’s disease.
- As treatments for dementia emerge, these tests will help doctors deliver the right treatment in the right place at the right time to patients.
Stroke Awareness
Each year in the U.S. people have more than 800,000 strokes. NIH has worked to increase public awareness around stroke through the Know Stroke campaign, which has reached millions of people.
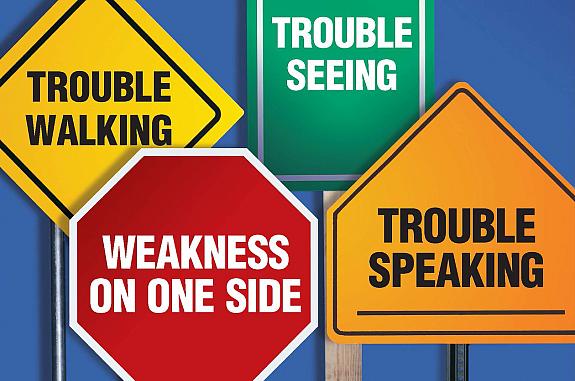
Image credit: National Institute of Neurological Disorders and Stroke, NIH
- Stroke is a leading cause of death in the U.S. and is a major cause of serious disability for adults.
- NIH developed the Know Stroke. Know the Signs. Act in Time. campaign to help educate the public about the symptoms of stroke and the importance of getting to the hospital quickly. NIH also launched the related Mind Your Risks® campaign, focused on blood pressure control for the prevention of stroke and dementia.
- These campaigns include public outreach using mass media, grassroots outreach, partnerships, and community education.
Stroke Treatment
NIH played a major role in the development of the clot-busting medicine tissue plasminogen activator (tPA), which was the first treatment for strokes caused by blood clots and remains a frontline therapy. Approved by FDA in 1996, tPA transformed stroke care to enable rapid intervention and was an impetus for future treatments.
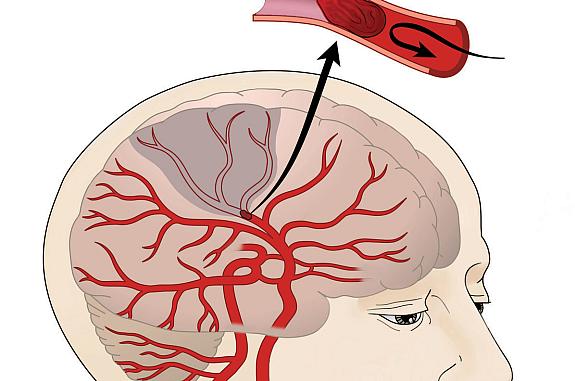
Image credit: National Institute of Neurological Disorders and Stroke, NIH
- Ischemic stroke is caused by the blockage of a vessel supplying blood to the brain.
- When administered quickly after stroke onset, tPA helps to restore blood flow to brain regions affected by an ischemic stroke, limiting the risk of damage and impairment.
- Hundreds of hospitals around the U.S. now have resources and protocols to rapidly diagnose a stroke with brain imaging and administer tPA.
- NIH research also contributed to the development of endovascular thrombectomy (EVT), a minimally invasive surgery to treat ischemic stroke up to 24 hours after a stroke starts, long after tPA can be effective.
References
Couples Therapy
- Preventing Intimate Partner Violence Across the Lifespan: A Technical Package of Programs, Policies, and Practices: https://www.cdc.gov/violenceprevention/pdf/ipv-technicalpackages.pdf
- Braithwaite SR, et al. Behav Res Ther. 2014;54:12-21. PMID: 24463577.
Obsessive Compulsive Disorder
- Law C, et al. Psychol Res Behav Manag. 2019;12:1167-1174. PMID: 31920413.
- Foa EB. Dialogues Clin Neurosci. 2010;12(2):199-207. PMID: 20623924.
- Abramowitz JS. Can J Psychiatry. 2006;51(7):407-16. PMID: 16838822.
- Motivala SJ, et al. Int J Psychiatry Clin Pract. 2018;22(1):40-46. PMID: 28691550.
- Foa EB, et al. Am J Psychiatry. 2005;162(1):151-61. PMID: 15625214.
- Obsessive-Compulsive Disorder: https://www.nimh.nih.gov/health/topics/obsessive-compulsive-disorder-ocd
- Obsessive-Compulsive Disorder and Substance Use Disorders: https://store.samhsa.gov/sites/default/files/d7/priv/sma16-4977.pdf
- Strauss C, et al. J Anxiety Disord. 2018;57:39-47. PMID: 29739634.
Phobias
- Choy Y, et al. Clin Psychol Rev. 2007;27(3):266-86. PMID: 17112646.
- Craske MG, et al. Behav Res Ther. 2014;58:10-23. PMID: 24864005.
- Zlomke K, et al. Behav Ther. 2008;39(3):207-23. PMID: 18721635.
- Raeder F, et al. Sci Rep. 2020;10(1):4288. PMID: 32152429.
Depression
- Dimidjian S, et al. J Consult Clin Psychol. 2006;74(4):658-70. PMID: 16881773.
- Kessler RC, et al. Arch Gen Psychiatry. 2005;62(6):593-602. PMID: 15939837.
- Results from the 2013 National Survey on Drug Use and Health: Mental Health Findings: https://www.samhsa.gov/data/sites/default/files/NSDUHmhfr2013/NSDUHmhfr2013.pdf
Psychosis
- Kane J, et al. American Journal of Psychiatry 2016; 173(4):362-372. PMID: 26481174.
- Addington J, et al. Psychiatric Services 2015;66(7):753-756. PMID: 25588418.
- Marino L, et al. Early Interv Psychiatry 2020;14:544-52. PMID: 31502409.
- Substance Abuse and Mental Health Services Administration. 2021 Uniform Reporting System (URS) Output Tables. 2022. Available at https://www.samhsa.gov/data/report/2021-uniform-reporting-system-urs-output-tables
Addiction Treatment
- Article: A Scientific Discovery Revolutionizes Our View of Addiction: https://www.bbrfoundation.org/content/scientific-discovery-revolutionizes-our-view-addiction
- Volkow ND, et al. N Engl J Med. 2016;374(4):363-71. PMID: 26816013.
- Leshner AI. Science. 1997;278(5335):45-7. PMID: 9311924.
- McGinty EE, et al. Health Aff (Millwood). 2015;34(8):1331-9. PMID: 26240247.
- Government Accountability Office: Mental Health and Substance Use: Employers’ Insurance Coverage Maintained or Enhanced Since Parity Act, but Effect of Coverage on Enrollees Varied. 2011. https://www.gao.gov/assets/gao-12-63.pdf
Mood Stabilizers
- Goodwin FK. Arch Gen Psychiatry. 1969;21(4):486-96. PMID: 4896983.
- The Veterans Administration/Department of Defense. Clinical Practice Guideline for Management of Bipolar Disorder in Adults. 2010. https://www.healthquality.va.gov/guidelines/MH/bd/bd_306_sum.pdf
- Bipolar Disorder: https://www.nimh.nih.gov/health/topics/bipolar-disorder
Deep Brain Stimulation
- Deep Brain Stimulation for Movement Disorders: https://www.ninds.nih.gov/health-information/disorders/deep-brain-stimulation-movement-disorders
- Deep brain stimulation (DBS) for the treatment of Parkinson’s disease and other movement disorders: https://www.ninds.nih.gov/about-ninds/impact/ninds-contributions-approved-therapies/deep-brain-stimulation-dbs-treatment-parkinsons-disease-and-other-movement-disorders
- Neurostimulation Technologies Harnessing Electricity to Treat Lost Neural Function: https://www.nih.gov/sites/default/files/about-nih/impact/neurostimulation-technologies-case-study.pdf
- Weaver FM, et al. JAMA. 2009;301(1):63-73. PMID: 19126811.
- Vitek JL, et al. Lancet Neurol. 2020;19(6):491-501. PMID: 32470421.
- Indications for Medtronic DBS: http://professional.medtronic.com/pt/neuro/dbs-md/eff/data-and-clinical-outcomes
- Rizzone MG, et al. Parkinsonism Relat Disord. 2014;20(4):376-81. PMID: 24508574.
- Bove F, et al. Neurology. 2021:10.1212/WNL.0000000000012246. PMID: 34078713.
- Article: Self-tuning brain implant could help treat patients with Parkinson’s disease: https://www.nih.gov/news-events/news-releases/self-tuning-brain-implant-could-help-treat-patients-parkinsons-disease
- Article: Researchers wirelessly record human brain activity during normal life activities: https://www.ninds.nih.gov/news-events/news/press-releases/researchers-wirelessly-record-human-brain-activity-during-normal-life-activities
- GBD 2016 Parkinson's Disease Collaborators. Lancet Neurol. 2018;17(11):939-953. PMID: 30287051.
- Vedam-Mai V, et al. Front Hum Neurosci. 2021;15:644593. PMID: 33953663.
- Humanitarian Device Exemption for Medtronic (Activa)Deep Brain Stimulation for OCD Therapy: https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfhde/hde.cfm?id=H050003
Dementia Biomarkers
- Alzheimer's Disease & Related Dementias: https://www.nia.nih.gov/health/alzheimers
- Video: Biomarkers and How They Help Diagnose Dementia: https://www.youtube.com/watch?v=n5m_qOy14VQ
- How Biomarkers Help Diagnose Dementia: https://www.nia.nih.gov/health/how-biomarkers-help-diagnose-dementia
- Biomarkers: https://www.nia.nih.gov/news/topics/biomarkers
- Article: Small Business Spotlight: C₂N Diagnostics’ blood test detects Alzheimer’s: https://www.nia.nih.gov/news/small-business-spotlight-c2n-diagnostics-blood-test-detects-alzheimers
- PrecivityAD™ blood test: https://precivityad.com/news/alzheimers-breakthrough
Stroke Awareness
- Know Stroke: Know The Signs. Act In Time.: https://www.stroke.nih.gov
- 2.Tissue Plasminogen Activator for Acute Ischemic Stroke: https://www.ninds.nih.gov/about-ninds/impact/ninds-contributions-approved-therapies/tissue-plasminogen-activator-acute-ischemic-stroke-alteplase-activaser
- CDC Stroke:https://www.cdc.gov/stroke/
- Mind Your Risks®: https://www.mindyourrisks.nih.gov
Stroke Treatment
- Tissue Plasminogen Activator for Acute Ischemic Stroke: https://www.ninds.nih.gov/about-ninds/impact/ninds-contributions-approved-therapies/tissue-plasminogen-activator-acute-ischemic-stroke-alteplase-activaser
- Lees KR, et al. Stroke. 2016;47(9):2373-9. PMID: 27507856.
- Joo H, et al. Stroke Vasc Neurol. 2017;2(2):73-83. PMID: 28736623.
- Tung CE, et al. Stroke. 2011;42(8):2257-62. PMID: 21719767.
- Johnston SC. Stroke. 2010;41(10 Suppl):S59-62. PMID: 20876507.
- Demaerschalk BM, et al. Stroke. 2005;36(11):2500-3. PMID: 16224087.
- Boudreau DM, et al. Stroke. 2014;45(10):3032-9. PMID: 25190439.
- Fagan SC, et al. Neurology. 1998;50(4):883-90. PMID: 9566367.
- Optimizing endovascular therapy for ischemic stroke: https://www.ninds.nih.gov/about-ninds/what-we-do/impact/ninds-contributions-approved-therapies/optimizing-endovascular-therapy-ischemic-stroke
This page last reviewed on March 28, 2025