Probiotic blocks staph bacteria from colonizing people
February 7, 2023
Probiotic blocks staph bacteria from colonizing people
At a Glance
- A probiotic reduced the amount of Staphylococcus aureus, or “staph,” bacteria in the human gut and nose without harming beneficial gut microbes.
- The results suggest a way to prevent dangerous S. aureus infections without antibiotics.
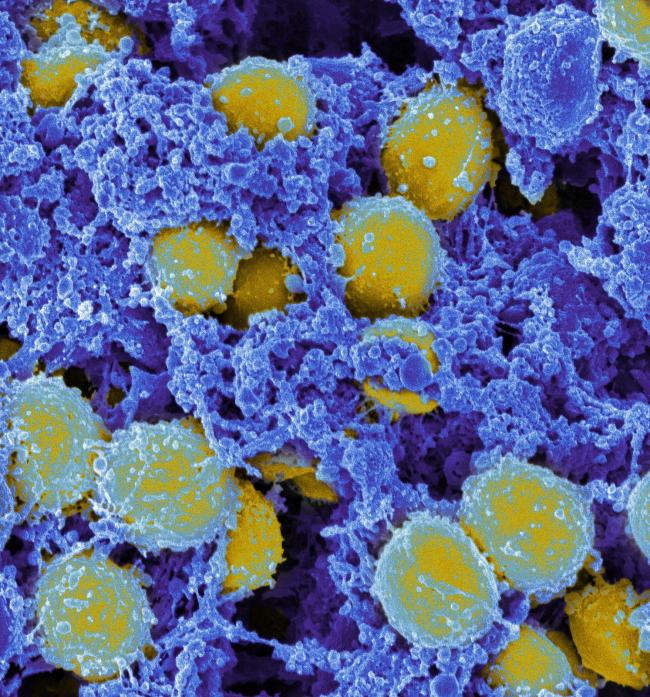
Antibiotic-resistant bacteria have become a major public health threat. The deadliest such pathogen in the United States is Staphylococcus aureus. Serious and even fatal infections occur when the bacteria get into the blood, lungs, bone, or lower layers of the skin. But S. aureus can also live in the nose, on the skin surface, and in the gut without causing any harm. Many S. aureus infections begin as this symptom-free colonization, which may occur in a quarter to a third of the population.
Decolonization—eliminating the symptom-free bacteria—could prevent harmful S. aureus infections. Previous decolonization strategies have used topical antibiotics or antiseptics to get rid of S. aureus from the nose or skin. These efforts have had limited success, likely because they don’t affect S. aureus in the gut. Decolonizing the gut would require oral antibiotics. But this risks harming the beneficial gut microbes that usually help prevent infections. It could also lead to more antibiotic resistance.
In previous work, an international research team led by Dr. Michael Otto at NIH’s National Institute of Allergy and Infectious Diseases (NIAID) found that another species of bacteria, Bacillus subtilis, secretes molecules that inhibit S. aureus colonization. An oral probiotic containing live B. subtilis spores eliminated S. aureus from the guts of mice. This suggested that probiotics might decolonize S. aureus from the human gut without the risks that go with antibiotics.
The researchers tested this strategy by conducting a clinical trial in Thailand with collaborators from Rajamangala University of Technology Srivijaya and Prince of Songkla University. The team screened more than 600 people and found 115 who had S. aureus in their gut, nose, or both. These were assigned at random to take either a B. subtilis probiotic or placebo daily for four weeks. Results appeared in Lancet Microbe on February 1, 2023.
After four weeks of probiotic treatment, S. aureus in the stool, a proxy for gut S. aureus, declined by 97%. S. aureus in the nose declined by 65%. Between the effects on these two sites, the researchers estimated that probiotic treatment got rid of at least 95% of S. aureus in the human body. In the people getting placebo treatment, S. aureus numbers did not change in either the gut or nose. The team found no other changes in microbiome composition among people who took the probiotic. They also saw no differences in side effects between the treatment and placebo groups.
The results suggest that B. subtilis probiotics could safely reduce S. aureus colonization in the human body. Such a strategy could help lower infection rates, particularly in high-risk settings such as nursing homes. This study also demonstrates the importance of targeting the gut for S. aureus decolonization in general. Decolonizing the gut led to a large reduction in S. aureus throughout the body. In contrast, decolonizing the nose only affects a small part of the body's total S. aureus.
“The probiotic we use does not ‘kill’ S. aureus, but it specifically and strongly diminishes its capacity to colonize,” Otto says. “We think we can target the ‘bad’ S. aureus while leaving the composition of the microbiota intact.”
Related Links
- Compound Produced by Bacteria Protects the Skin
- Bacteria Therapy Improves Eczema in Children
- Probiotic Bacteria Block Harmful Microbe
- Bacteria Therapy Tested for Common Skin Disease
- Probiotic Prevents Infant Infections in Rural India
- Antibiotic Combinations May Combat MRSA Infections
- Molecular Insights into a Target for Multidrug Resistance
- New Drug Effective Against MRSA in Mice
- Your Body’s Bugs
- Probiotics: What You Need to Know
References
Probiotic for pathogen-specific Staphylococcus aureus decolonisation in Thailand: a phase 2, double-blind, randomised, placebo-controlled trial. Piewngam P, Khongthong S, Roekngam N, Theapparat Y, Sunpaweravong S, Faroongsarng D, Otto M. Lancet Microbe. 2023 Feb;4(2):e75-e83. doi: 10.1016/S2666-5247(22)00322-6. Epub 2023 Jan 13. PMID: 36646104.
Funding
NIH’s National Institute of Allergy and Infectious Diseases (NIAID); National Research Council of Thailand.


