You are here
August 10, 2021
Detergent-like protein kills bacteria in human cells
At a Glance
- Researchers identified a protein that acts like a detergent to kill bacteria inside human cells.
- The findings reveal a previously unknown defense mechanism against bacteria and could lead to new antibacterial treatments.

Many of the body’s defenses against infections operate outside of host cells. But some bacterial pathogens can hide inside host cells to avoid these defenses. To help catch these intracellular lurkers, immune cells secrete a molecular signal called interferon-gamma (IFN-γ). In addition to stimulating immune cells, IFN-γ also prompts non-immune cells to activate, or express, many genes. This leads to the death of the invading bacteria, but researchers haven’t been sure how this occurs.
A team led by Dr. John MacMicking, a Howard Hughes Medical Institute Investigator at Yale University School of Medicine, explored which products of IFN-γ-stimulated genes might kill bacteria inside the host cell. NIH’s National Institute of Allergy and Infectious Diseases (NIAID) and National Institute of Neurological Disorders and Stroke (NINDS) supported the research. Results appeared in Science on July 16, 2021.
The team infected cultured human cells with a strain of Salmonella, which can replicate within host cells. Salmonella belongs to a class of bacteria that have two cell membranes, which protects against many antibiotics. Exposing the cells to IFN-γ hindered the bacteria’s ability to replicate within the cells.
The team then used CRISPR gene-editing techniques to disable various genes in the human cells. They looked for genes whose expression was stimulated by IFN-γ and that led to increased bacterial replication when disabled. The apolipoprotein L3 (APOL3) gene met both criteria. Silencing APOL3 expression allowed Salmonella to replicate in various cell types. These included cells from the lining of the intestines and blood vessels and from connective tissues.
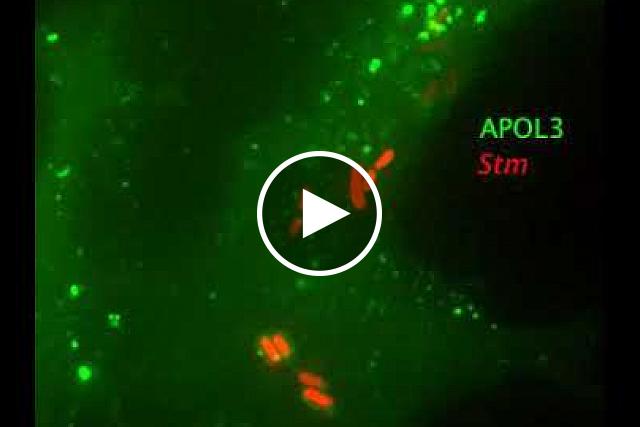
APOL3 belongs to a group of six genes; the functions of most are unknown. Under a microscope, the team observed APOL3 protein coating the surface of Salmonella bacteria. Within hours, APOL3 penetrated the bacterial cell membranes.
When Salmonella (red) invades a cell, APOL3 (green) gloms on to the bacterium’s surface and breaks it apart. R. Gaudet et al./Science 2021
To better understand how APOL3 interacts with cell membranes, the researchers created artificial membranes that resembled bacterial membranes. Cell membranes consist of oily molecules called lipids that don’t dissolve in water. APOL3 acted like a detergent, working with other proteins to break up the lipids and dissolve the membranes. Disabling APOL3’s ability to dissolve cell membranes also destroyed its ability to kill Salmonella. Cholesterol, which animal cell membranes contain but bacterial membranes lack, inhibited membrane breakdown. Thus, APOL3 attacked bacterial membranes while avoiding the host cell membranes.
These findings reveal how non-immune cells defend against infections. They also identify a novel mechanism used by the body to kill bacteria. The researchers note that they are still a long way from being able to develop therapies based on these results. But MacMicking hopes that the findings could one day lead to improved tools for fighting infections.
“This is a case where humans make their own antibiotic in the form of a protein that acts like a detergent,” he says. “We can learn from that.”
—by Brian Doctrow, Ph.D.
Related Links
References: A human apolipoprotein L with detergent-like activity kills intracellular pathogens. Gaudet RG, Zhu S, Halder A, Kim BH, Bradfield CJ, Huang S, Xu D, Mamiñska A, Nguyen TN, Lazarou M, Karatekin E, Gupta K, MacMicking JD. Science. 2021 Jul 16;373(6552):eabf8113. doi: 10.1126/science.abf8113.
Funding: NIH’s National Institute of Allergy and Infectious Diseases (NIAID) and National Institute of Neurological Disorders and Stroke (NINDS); National Health and Medical Research Council; Australian Research Council; Howard Hughes Medical Institute; Helen Hay Whitney Foundation.