You are here
Backgrounder: NIH Collaboration on Gene-Based Cures for SCD and HIV
Overview of SCD and HIV Cures Collaboration
- The National Institutes of Health launched a new collaboration to fund research that may lead to curative strategies for sickle cell disease (SCD) and HIV using gene-based treatments.
- Initially, the NIH plans to invest at least $100 million over the next four years to advance accessible and scalable candidate interventions. The Bill & Melinda Gates Foundation will also invest $100 million and the collaboration will leverage the organizations’ collective strengths in basic and translational science for gene-based technologies and efforts to combat diseases that have a major public health impact.
- The collaboration aims to produce gene-based candidate treatments for SCD and HIV that can be administered at scale via low-cost delivery systems and advance them toward clinical trials in the United States and in Africa for safety and effectiveness within the next seven to 10 years.
- The collaboration will focus on two areas of coordination with a focus on advancing the science on gene-based strategies that are common to both SCD and HIV:
- First, identify potential cure candidates for SCD and HIV for pre-clinical and clinical evaluation, co-funded by the NIH and Gates Foundation
- Second, define long-term opportunities to work together on advancing promising candidates to late-phase clinical trials, with funding and inclusion of other partners to be determined as candidates progress
- Both organizations also will continue to invest in parallel research on cures for SCD and HIV outside of this collaboration.
The Potential of Gene-Based Treatments
- Gene therapy is a technique that uses genes to prevent or treat a disease. This can include replacing or inactivating a disease-causing gene or introducing a new or modified gene to help treat a disease.
- Gene editing is a technique that uses different technologies to modify DNA at a specific spot, allowing scientists to remove, add or replace the DNA where it was cut in order to correct a genetic defect.
- After dramatic changes in genetic science over the past decade, fueled by advances in gene delivery and expression technology and novel gene editing mechanisms, gene-based approaches are being used to successfully treat some genetic diseases and cancers. Between the U.S. Food and Drug Administration and the European Medicines Agency, six gene therapy products have been approved since 2016 and more than 800 cell- and gene-based therapies are currently in clinical development.
- Recently, NIH studies demonstrated the effectiveness of correcting defective genes outside the body and infusing them into the body of SCD patients to reverse the disease.
- These are tremendous breakthroughs, but they are time intensive and involve multiple complicated manufacturing and clinical steps. Thus, gene-based approaches are currently only available in high-resource settings and cannot be scaled up to help solve public health problems on a broad scale.
- This collaboration aims to change this treatment landscape by accelerating research on gene-based interventions for SCD and HIV.
- Though SCD, a heritable disease, and HIV, an acquired disease, present significantly different scientific challenges, gene-based treatments hold promise for both, and many of the technical challenges for developing scalable gene-based cures are expected to be common to both diseases.
- An effective gene-based intervention for SCD would correct the gene mutations that cause the disease or, alternatively, promote the production of normal red blood cells in sufficient quantity to ward off symptoms. For HIV, an effective gene-based treatment would safely modify selected cells to stop the virus from replicating, eliminate it from the body, and prevent re-infection.
Background on SCD and Current Therapeutic Approaches
Overview
- SCD is a genetic condition that presents in infancy. Mutations in the gene for beta globin, a component of hemoglobin, cause red blood cells to become hard, sticky, and misshapen in the form of a C-shaped “sickle.” Sickle cells die early, causing a constant shortage of red blood cells, and can clog blood flow, resulting in pain and other serious problems.
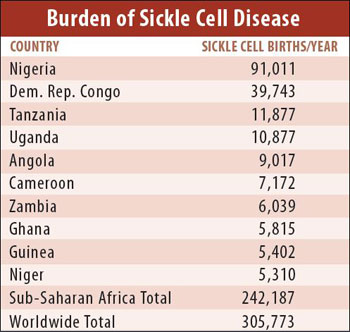
- SCD affects millions of people and is particularly common across sub-Saharan Africa.
- An estimated 300,000 children are born each year with SCD, about two‐thirds of them in Africa. Between 50-90 percent of infants born with SCD in developing nations will die before their fifth birthday. Nigeria, Tanzania and the Democratic Republic of the Congo bear the majority of Africa's SCD burden.
- Within the United States, SCD affects approximately 100,000 people, mostly within African American and Hispanic American communities.
- SCD occurs in approximately 1 out of every 365 black or African American births. Living with SCD typically requires frequent blood transfusions, hospitalizations and complication management.
Current Therapeutic Approaches
- Treatments are available that can prevent complications, relieve symptoms and lengthen the lives of SCD patients.
- For children, one of the most effective strategies for reducing mortality has been screening, caregiver education and pneumococcal prophylaxis. However, there remains a shortage of such programs in Africa and other resource-limited settings due to the high cost of screening, limited health system infrastructure and lack of affordable treatment options.
- In high-income settings, living with SCD typically requires frequent hospitalizations and complication management. Blood transfusions can be used to treat severe anemia or reduce the risk of stroke.
- Currently, the only cure for SCD is through stem cell or bone marrow transplant, though some gene therapy approaches have cured several patients in the United States. Bone marrow transplantation infuses healthy stem cells into the body to replace diseased bone marrow. While these transplants are increasingly used to successfully cure SCD, they require a matched donor and can cause severe side effects.
Background on HIV and Current Therapeutic Approaches
Overview
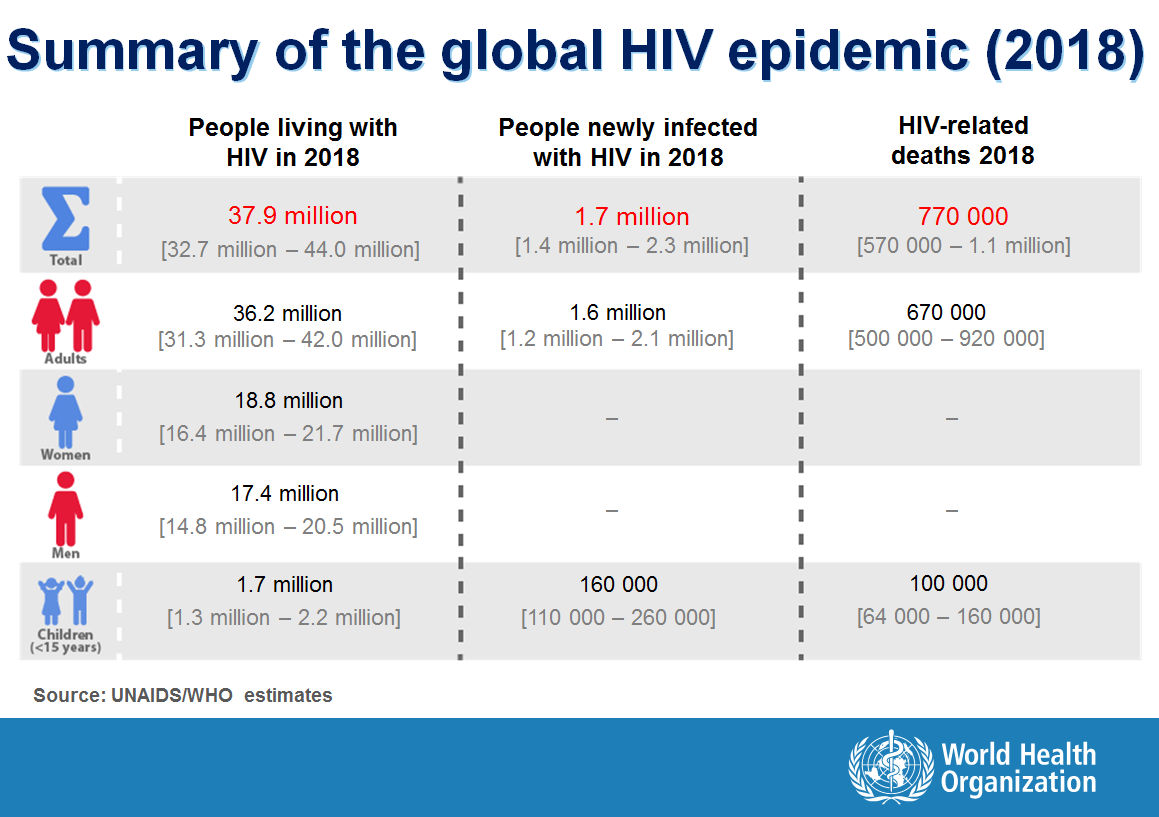
- Nearly 38 million people worldwide are living with HIV, with 770,000 AIDS-related deaths in 2018 alone.
- Africa is the continent most severely affected by HIV and AIDS. Nearly 26 million people in sub-Saharan Africa are living with HIV, accounting for more than two-thirds of the people living with HIV worldwide.
- In the United States, an estimated 1.1 million people are living with HIV, with nearly 39,000 people receiving a new HIV diagnosis in 2017.
- In the United States, men who have sex with men are disproportionately impacted, accounting for two-thirds of all HIV diagnoses. Black/African-Americans and Latinx individuals are disproportionately affected.
Current Therapeutic Approaches:
- Major strides have been made in treating people living with HIV in both high- and low-income settings around the world. HIV treatment consists of a combination of drugs, known as antiretroviral therapy (ART), that can be delivered in a single pill taken daily. ART has transformed HIV from an almost uniformly fatal disease into a manageable chronic condition. Starting daily antiretroviral therapy as soon as possible after diagnosis and staying on treatment are essential for keeping HIV under control, benefiting individual health and preventing sexual transmission to others. ART is recommended for all people with HIV, regardless of how long they’ve had the virus.