Dysfunctional exosomes involved in chronic inflammation in diabetic wounds
October 3, 2023
Dysfunctional exosomes involved in chronic inflammation in diabetic wounds
At a Glance
- Tiny signaling particles called exosomes isolated from the chronic wounds of people with diabetes were dysfunctional and promoted inflammation.
- Restoring functional exosomes may be a strategy to resolve chronic inflammation and help wounds in people with diabetes to heal.
In diabetes, levels of blood glucose, also called blood sugar, are too high. Over time, this can lead to many health problems, including a reduced ability of the skin to heal after injury. Foot ulcers, a type of chronic, non-healing wound, are a major cause of lower limb amputations, disability, and death in people with diabetes.
The processes that interfere with the normal healing process in people with diabetes remain incompletely understood. Recently, interest has grown in the role of exosomes in wound healing. Exosomes are nanosized, fluid-filled sacs released from cells that can carry cargo like proteins, peptides, and messenger RNA. They play an important role in communication between cells.
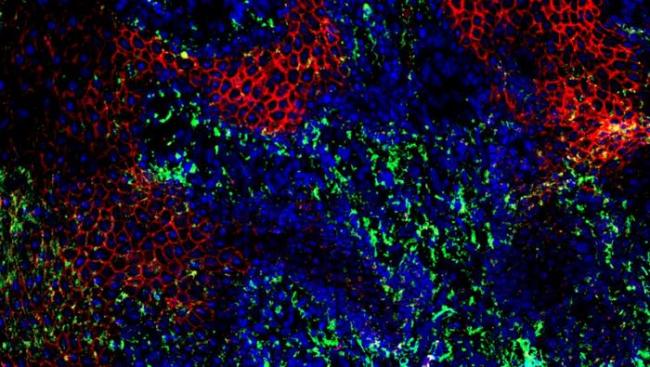
An NIH-funded research team led by Drs. Chandan Sen and Subhadip Ghatak from the University of Pittsburgh has been studying the role of exosomes in inflammation, which is a problem in chronic diabetic wounds. They have focused on the exosomes produced by keratinocytes, a common type of skin cell vital for wound healing and maintaining the barrier function of skin.
In their new study, they compared exosomes isolated from chronic wounds in 22 people with diabetes with those from wounds in 15 people without diabetes. The results were published in the October 2023 issue of Nano Today.
The team first developed a process to isolate keratinocyte-derived exosomes in wound fluid. This process was based primarily on marker proteins that are uniquely found in keratinocytes. The researchers found that their new method could distinguish exosomes released by keratinocytes from other exosomes with very high accuracy. Using the new method, the team calculated that exosomes from keratinocytes made up about a quarter of the total exosomes in chronic wound fluid.
Further experiments revealed that these exosomes differed substantially in the chronic wounds of people with and without diabetes. Fewer exosomes were isolated from people with diabetes, and these were dysfunctional. They contained less RNA than normal and were deficient in proteins and fats needed for the exosomes to function normally.
The researchers next tested the exosomes in laboratory experiments with macrophages, a type of immune cell needed for wound healing. Macrophages exposed to the keratinocyte exosomes from non-diabetic patients showed signs of the resolution of inflammation. In contrast, macrophages exposed to those from people with diabetes stayed in a persistent inflammatory state, similar to that seen in people with diabetic ulcers. These exosomes also attracted additional macrophages towards them. In the body, this would lead to persistent inflammation and a breakdown in the healing process.
“If incoming keratinocyte signals contained within exosomes are correct, the macrophage knows how to resolve inflammation in the wound,” Sen explains. “In diabetes, crosstalk between keratinocytes and macrophages is compromised, so macrophages keep driving inflammation and the wound can’t heal.”
The researchers are planning future studies to see if exosomes can be engineered to restore the ability to promote wound healing in people with diabetes.
—by Sharon Reynolds
Related Links
- Smart Bandage Improves Wound Healing in Mice
- Newly Identified Oral Stem Cell Key to Wound Healing
- Brain Cells That Influence Aging
- Biomarkers for Early Organ Transplant Rejection
- To Heal a Wound: Helping the Skin Fix Itself
- Diabetes
References
Nanoscopic and functional characterization of keratinocyte-originating exosomes in the wound fluid of non-diabetic and diabetic chronic wound patients. Guda et al. nanotoday. Volume 52, October 2023, 101954. https://doi.org/10.1016/j.nantod.2023.101954.
Funding
NIH’s National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK); Indiana Center for Regenerative Medicine and Engineering.


