Gut cells distinguish between sugar and artificial sweeteners
February 1, 2022
Gut cells distinguish between sugar and artificial sweeteners
At a Glance
- Researchers found cells in the small intestines of mice that communicate with the brain and influence the preference for sugar over artificial sweeteners.
- The technology developed for the study may help decipher how the brain responds to nutrients and how their intake affects appetite.
Animals, including humans, have evolved to enjoy sweet foods. This preference encouraged people to seek out high-calorie foods to help them survive. But in the present, with an excess of calories available, it contributes to obesity and associated health problems.
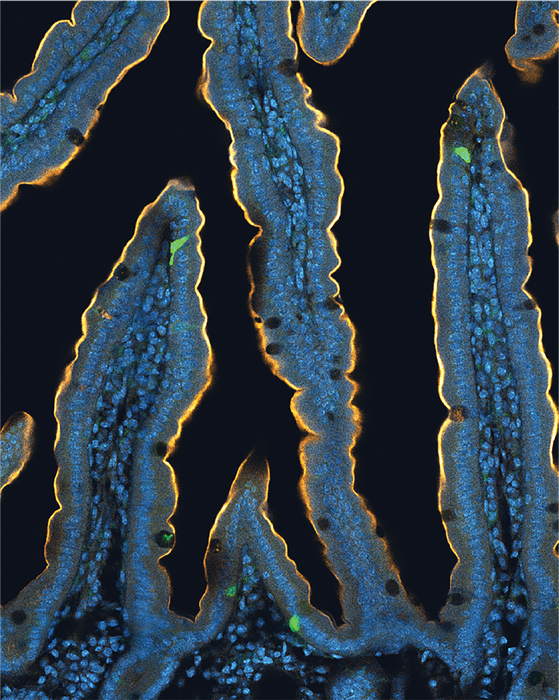
Studies have found that a “sweet tooth” doesn’t involve just the taste buds on the tongue. The upper part of the small intestine, the duodenum, also appears to play an important role in sensing and craving sugar.
Recent research from the laboratory of Dr. Diego Bohórquez at Duke University uncovered direct neural connections between the gut and the brain. These connections form between the vagus nerve, which stretches from the brain all the way to the intestines, and cells in the gut called enteroendocrine or neuropod cells. Such connections allow information to travel between the gut and the brain in fractions of a second.
To see if neuropod cells play a role in the body’s preference for sugar, the team performed a new set of experiments in cells and mice. They measured differences in activity in neuropod cells after exposure to sugar or artificial sweeteners such as sucralose. The researchers also developed an experimental tool based on a technology called optogenetics. It used a tiny fiberoptic cable that allowed them to manipulate the activity of neuropod cells in living mice. They could then observe the resulting changes in feeding behavior.
The new study was funded in part by NIH’s National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), National Center for Complementary and Integrative Health (NCCIH), and National Institute of Mental Health (NIMH). Results were published on January 13, 2022, in Nature Neuroscience.
Both sugar and artificial sweeteners delivered directly into mouse small intestines activated the vagus nerve. But different types of neuropod cells responded to different types of sweet stimuli. Further experiments showed that these different cells used different neurotransmitters to communicate with distinct sets of neurons in the vagus nerve. The brain therefore received different signals after consumption of sugar or artificial sweeteners.
The team used their optogenetic system to temporarily turn off the neuropod cells that sense sugar in mice. When these cells were blocked from signaling to the vagus nerve, mice lost their preference for sugar and became equally likely to choose artificial sweeteners.
When the researchers turned the sugar-sensing neuropod cells back on, the mice once again preferred sugar. Similar results were seen when the team used drugs to block the neurotransmitter that the sugar-sensing neuropod cells use to communicate with the vagus nerve.
“Many people struggle with sugar cravings, and now we have a better understanding of how the gut senses sugars and why artificial sweeteners don’t curb those cravings,” says Dr. Kelly Buchanan, who helped lead the study.
The optogenetic technology developed for this work could now be used to further explore how these different signaling pathways affect energy balance and body weight. The approach could also potentially be used to study how other nutrients, such as fat and protein, are sensed by the brain and help drive appetite.
—by Sharon Reynolds
Related Links
- Gut Communicates Directly with Brain
- How Fructose May Contribute to Obesity and Cancer
- How High Fructose Intake May Trigger Fatty Liver Disease
- High Blood Sugar May Blunt Benefits of Aerobic Exercise
- Sweet Stuff: How Sugars and Sweeteners Affect Your Health
- Diet & Nutrition
References
The preference for sugar over sweetener depends on a gut sensor cell. Buchanan KL, Rupprecht LE, Kaelberer MM, Sahasrabudhe A, Klein ME, Villalobos JA, Liu WW, Yang A, Gelman J, Park S, Anikeeva P, Bohórquez DV. Nat Neurosci. 2022 Jan 13. doi: 10.1038/s41593-021-00982-7. Online ahead of print. PMID: 35027761.
Funding
NIH’s National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), National Center for Complementary and Integrative Health (NCCIH), and National Institute of Mental Health (NIMH); Howard Hughes Medical Institute; Hartwell Foundation; McGovern Institute; Yang-Tan Neuroscience Centers; Duke-NUS Medical School.


