How SARS-CoV-2 contributes to heart attacks and strokes
October 24, 2023
How SARS-CoV-2 contributes to heart attacks and strokes
At a Glance
- SARS-CoV-2 infected coronary arteries and increased inflammation in atherosclerotic plaques.
- The findings suggest how COVID-19 could increase the risk of heart attack and stroke.
COVID-19 is known to increase the risk of heart attack and stroke. The intense inflammation that occurs throughout the body in severe cases likely contributes to this increased risk. But it’s not clear whether SARS-CoV-2, the virus that causes COVID-19, also affects blood vessels directly.
To find out, an NIH-funded research team, led by Dr. Chiara Giannarelli at New York University School of Medicine, analyzed coronary artery tissue samples from eight people who died of COVID-19 between May 2020 and May 2021. Results appeared in Nature Cardiovascular Research on September 28, 2023.
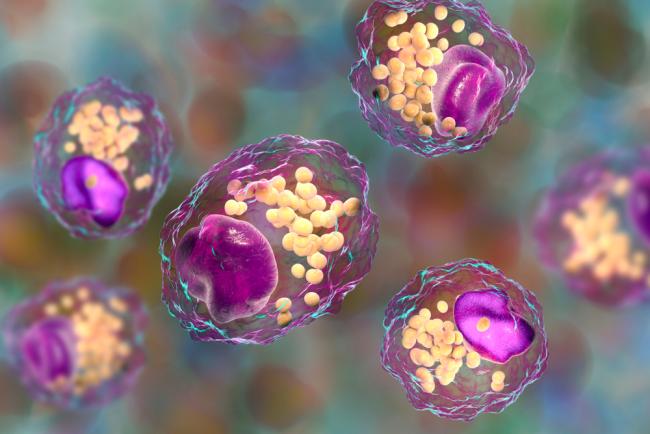
The team found SARS-CoV-2 viral RNA in coronary artery tissue from all patients. They found more viral RNA in the arterial walls than in the surrounding fat tissue. Many of the infected cells were macrophages, a type of white blood cell that ingests pathogens. Samples with more macrophages had more viral RNA.
Macrophages also help remove cholesterol from blood vessels. When macrophages become laden with cholesterol, they are known as foam cells. Accumulation of foam cells within arteries forms plaques that are a hallmark of atherosclerosis. The team confirmed that SARS-CoV-2 could infect human macrophages and foam cells in a petri dish. The foam cells were much more susceptible to infection than the macrophages. This could explain why people with atherosclerosis are more vulnerable to COVID-19.
In both cell types, infection depended on a protein on the surface of the cells called neuropilin. Turning off the gene for neuropilin in these cells reduced infection. So did blocking the virus from binding to neuropilin.
Infection triggered several inflammatory pathways in macrophages and foam cells. The cells also released molecules that are known to contribute to heart attacks and strokes. In arterial plaques that had been surgically removed from patients, the researchers saw an inflammatory response to SARS-CoV-2 infection like that seen in the cultured cells.
The findings suggest that SARS-CoV-2 may increase the risk of heart attacks and stroke by infecting artery wall tissue, including associated macrophages. This provokes inflammation in atherosclerotic plaques, which could lead to heart attack or stroke.
“These results shed light onto a possible connection between preexisting heart issues and Long COVID symptoms,” Giannarelli says. “It appears that the immune cells most involved in atherosclerosis may serve as a reservoir for the virus, giving it the opportunity to persist in the body over time.”
“Since the early days of the pandemic, we have known that people who had COVID-19 have an increased risk for cardiovascular disease or stroke up to one year after infection,” says Dr. Michelle Olive of NIH’s National Heart, Lung, and Blood Institute. “We believe we have uncovered one of the reasons why.”
The authors plan to further investigate the potential link between infection of the arteries and Long COVID. They also aim to see if their results also hold true for newer SARS-CoV-2 variants.
—by Brian Doctrow, Ph.D.
Related Links
- Immune and Hormonal Features of Long COVID
- Long COVID Symptoms Linked to Inflammation
- SARS-Cov-2 Infection of The Inner Ear
- Autoimmune Response Found in Many With COVID-19
- Misdirected Antibodies Linked to Severe COVID-19
- Most COVID-19 Hospitalizations Due to Four Conditions
- How Disrupted Sleep May Lead to Heart Disease
- Understanding COVID-19
- COVID-19 Research
- Coronavirus Prevention Network
References
SARS-CoV-2 infection triggers pro-atherogenic inflammatory responses in human coronary vessels. Eberhardt N, Noval MG, Kaur R, Sajja S, Amadori L, Das D, Cilhoroz B, Stewart O, Fernandez DM, Shamailova R, Guillen AV, Jangra S, Schotsaert M, Gildea M, Newman JD, Faries P, Maldonado T, Rockman C, Rapkiewicz A, Stapleford KA, Narula N, Moore KJ, Giannarelli C. Nat Cardiovasc Res. 2023 Sep 28:2023.08.14.553245. doi: 10.1101/2023.08.14.553245. Preprint. PMID: 37645908.
Funding
NIH’s National Heart, Lung, and Blood Institute (NHLBI), National Center for Advancing Translational Sciences (NCATS), National Institute of Allergy and Infectious Diseases (NIAID), and National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK); American Heart Association; Chan Zuckerberg Initiative; New York University.


