How disrupted sleep may lead to heart disease
March 5, 2019
How disrupted sleep may lead to heart disease
At a Glance
- Researchers found that sleep disruption activates a molecule that triggers inflammation and leads to fatty buildup in mouse arteries.
- The findings underscore the importance of getting enough quality sleep to maintain heart health. It also suggests new targets for fighting heart disease.
Heart disease is the leading cause of death among women and men in the United States. The most common cause of heart disease is when fatty deposits called plaque build up inside your arteries, the blood vessels that carry oxygen-rich blood around your body. This is called atherosclerosis. White blood cells from the immune system collect at the plaque and cause inflammation.
Over time, the plaque hardens and narrows your arteries. This limits the flow of oxygen-rich blood to your heart and other organs. Atherosclerosis can lead to serious problems, including heart attack, stroke, or even death.
Recent research has linked sleep deficiency and certain sleep disorders, such as sleep apnea, to an increased risk of heart disease and other health conditions. But the molecular mechanisms underlying the link between sleep and heart disease has been unclear.
To learn more about the impact of sleep deficiency on heart disease, a team led by Dr. Filip Swirski at Harvard Medical School and Massachusetts General Hospital studied a group of mice that were genetically engineered to develop atherosclerosis. The research was supported in part by NIH’s National Heart, Lung, and Blood Institute (NHLBI). Results were published online on February 13, 2019, in Nature.
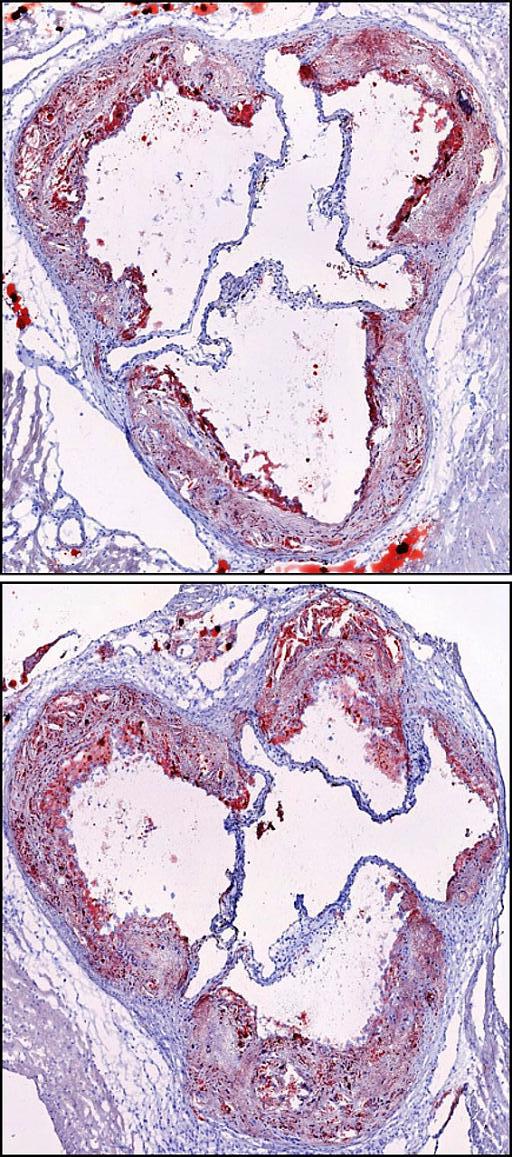
The researchers repeatedly disrupted the sleep cycles of half the mice, and the other half slept normally. After 16 weeks, the sleep-disrupted mice developed larger arterial plaques than the mice with normal sleep patterns.
The sleep-disrupted mice also had twice the level of certain white blood cells in their circulation than the control mice. And they had lower amounts of hypocretin, a hormone made by the brain that plays a key role in regulating sleep and wake states (also known as orexin). Further experiments showed that hypocretin suppressed the production of stem cells that make the white blood cells in their bone marrow.
Sleep-deficient mice that received hypocretin supplementation tended to produce fewer immune cells and develop smaller artery wall plaques than mice that weren’t given the supplementation. These results suggest that hypocretin loss during disrupted sleep contributes to inflammation and atherosclerosis.
“We’ve identified a mechanism by which a brain hormone controls production of inflammatory cells in the bone marrow in a way that helps protect the blood vessels from damage,” Swirski explains. “This anti-inflammatory mechanism is regulated by sleep, and it breaks down when you frequently disrupt sleep or experience poor sleep quality. It’s a small piece of a larger puzzle.”
“This appears to be the most direct demonstration yet of the molecular connections linking blood and cardiovascular risk factors to sleep health,” says Dr. Michael Twery, director of NHLBI’s National Center on Sleep Disorders Research.
If disrupted sleep proves to have similar effects in people, these findings could open new avenues for developing ways to treat heart disease.
Related Links
- Targeting Inflammation Molecules Reduces Heart and Liver Disease in Mice
- Sleep Deprivation Increases Alzheimer’s Protein
- How Sleep Clears the Brain
- Atherosclerosis
- Ischemic Heart Disease
- The Benefits of Slumber: Why You Need a Good Night’s Sleep
- Love Your Heart: Take Steps To Reduce Heart Risks
References
Sleep modulates haematopoiesis and protects against atherosclerosis.McAlpine CS, Kiss MG, Rattik S, He S, Vassalli A, Valet C, Anzai A, Chan CT, Mindur JE, Kahles F, Poller WC, Frodermann V, Fenn AM, Gregory AF, Halle L, Iwamoto Y, Hoyer FF, Binder CJ, Libby P, Tafti M, Scammell TE, Nahrendorf M, Swirski FK. Nature. 2019 Feb;566(7744):383-387. doi: 10.1038/s41586-019-0948-2. Epub 2019 Feb 13. PMID: 30760925.
Funding
NIH’s National Heart, Lung, and Blood Institute (NHLBI), American Heart Association, Massachusetts General Hospital, Swiss National Science Foundation, Government of Canada, Austrian Science Fund, Swedish Research Council, Fondation pour la Recherche Medicale, German Research Foundation, and Boehringer-Ingelheim-Fonds.


