Why protective antibodies fade after COVID-19 vaccines
October 29, 2024
Why protective antibodies fade after COVID-19 vaccines
At a Glance
- Researchers found that current COVID-19 vaccines fail to generate mature and durable antibody-producing cells in the bone marrow.
- The findings could help explain why protection tends to decline over time.
- Better understanding of long-term immune responses could lead to improved vaccines that provide enduring protection.
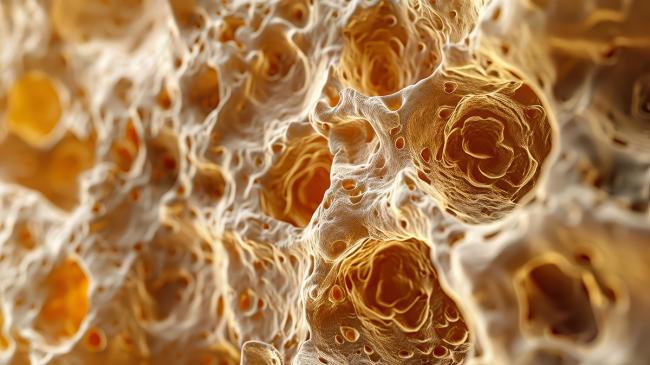
Some vaccines offer long-lasting protection. For instance, the tetanus vaccine provides protection for at least 10 years. With other vaccines, protection may begin to decline within a few months. To provide enduring immunity, a vaccine must elicit production of long-lived plasma cells, a type of immune cell that matures over time in the bone marrow and can rapidly trigger production of disease-fighting antibodies.
The mRNA vaccines developed for the SARS-CoV-2 virus have proven effective at preventing severe COVID-19 and reducing hospitalizations. These vaccines trigger production of antibodies that home in on the virus’s spike protein. But protective antibodies can begin to fade as soon as three months later and lead to breakthrough infections. Researchers have been puzzled by this waning protection, since SARS-CoV-2-specific immune cells can often be found in the bone marrow.
To better understand why protection against SARS-CoV-2 dwindles months after vaccination, a research team led by Dr. F. Eun-Hyung Lee of Emory University took a closer look at immune cells in the bone marrow of 19 healthy adults. Participants ranged in age from 20 to 65. All had previously received between two and five doses of mRNA COVID-19 vaccines. Samples of their bone marrow were evaluated within 33 months after receiving their initial COVID-19 vaccine shot.
The participants had also received an influenza vaccine within a year of giving their bone marrow samples. And all had previously received tetanus shots and boosters. Their responses to these previous vaccines were used for comparison.
The researchers used a cell-sorting technique called flow cytometry to separate each participant’s bone marrow immune cells into different groupings. These included short-lived antibody-secreting cells and long-lived plasma cells that confer lasting protection. Results appeared in Nature Medicine on September 27, 2024.
The scientists found that they could readily detect long-lived plasma cells that target tetanus and influenza. In contrast, while shorter-lived antibody-secreting cells specific to SARS-CoV-2 were abundant, long-lived ones were mostly absent. Even among five participants who had recent SARS-CoV-2 infections and vaccinations, long-lived plasma cells against the virus were scarce in the bone marrow samples.
The findings hint that newly created antibody-secreting cells against SARS-CoV-2 are unable to become fully mature and long-lasting once they reach and settle into the bone marrow. In contrast, vaccines against tetanus and influenza prompt antibody-producing cells to mature within bone marrow and become long-lived plasma cells. Future studies will need to investigate how to generate long-lived plasma cells against SARS-CoV-2.
“The holy grail of vaccine researchers is the generation of long-lived plasma cells,” Lee says. “Our findings demonstrate that current SARS-CoV-2 mRNA vaccines do not provide such long-lasting protection within bone marrow. Further research is needed to determine if updated vaccines, new delivery schedules, or other factors might provide such protection.”
—by Vicki Contie
Related Links
- How Boosters Produce Broad Protection Against COVID-19
- Fighting Current and Future Coronaviruses With a Single Vaccine
- T Cells Protect Against COVID-19 in Absence of Antibody Response
- Antibodies Recognize New SARS-CoV-2 Omicron Variant After Booster
- COVID-19 Immune Response Improves for Months After Vaccination
- COVID-19 Vaccines Induce Immune Response to Omicron
- Research in Context: Progress Toward Universal Vaccines
References
SARS-CoV-2-specific plasma cells are not durably established in the bone marrow long-lived compartment after mRNA vaccination. Nguyen DC, Hentenaar IT, Morrison-Porter A, Solano D, Haddad NS, Castrillon C, Runnstrom MC, Lamothe PA, Andrews J, Roberts D, Lonial S, Sanz I, Lee FE. Nat Med. 2024 Sep 27. doi: 10.1038/s41591-024-03278-y. Online ahead of print. PMID: 39333316.
Funding
NIH’s National Institute of Allergy and Infectious Diseases (NIAID), National Heart, Lung, and Blood Institute (NHLBI), and National Cancer Institute (NCI); Bill & Melinda Gates Foundation.


