Designing a new antibiotic to combat drug resistance
March 12, 2024
Designing a new antibiotic to combat drug resistance
At a Glance
- Researchers designed a synthetic drug that shuts down protein production in a range of different bacteria.
- The new antibiotic proved effective against drug-resistant bacterial strains in mice, but hasn’t yet been tested in people.
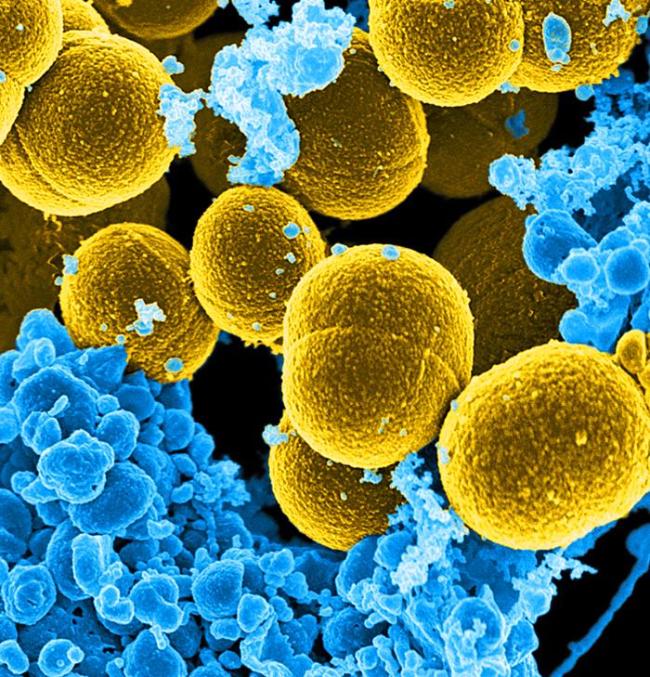
Antibiotic-resistant bacterial infections cause more than a million deaths worldwide every year. That number is expected to rise over the next decades unless new antibiotics can be developed.
Many antibiotics work by binding to and shutting down bacterial ribosomes. These are the molecular machines that build the proteins cells need to function. Over the last several decades, bacteria have evolved various mechanisms to prevent their ribosomes from being blocked by antibiotics. Often, genetic variants lead to changes in the chemical makeup of the ribosomes that prevent the antibiotics from binding.
A research team led by Dr. Andrew Myers from Harvard University, working with Dr. Yury Polikanov from the University of Illinois at Chicago, has been studying ways to tweak antibiotics to beat resistance. In a new study, funded in part by NIH, they examined an older class of antibiotic called lincosamides. Their results were published on February 16, 2024, in Science.
Lincosamide antibiotics are based on molecules found in nature, so are called semi-synthetic drugs. Using knowledge of the molecular structure of these antibiotics and how they bind to bacterial ribosomes, the team developed a fully synthetic compound called cresomycin. They chose its building blocks so that it would form the exact shape needed to latch tightly onto ribosomes.
The team found that cresomycin worked in both gram-positive and gram-negative bacteria. The latter are especially hard to treat with existing antibiotics. It also worked in strains resistant to other lincosamide antibiotics.
Using x-ray crystallography, the team explored how cresomycin overcomes the two most common resistance mechanisms that defeat other antibiotics. They obtained crystal structures of cresomycin in complex with two ribosomes that had been modified by different antimicrobial resistance genes. The structures revealed the tiny adjustments between the new antibiotic and the ribosomes that enabled tight binding.
The researchers next tested cresomycin in mice with antibiotic-resistant Staphylococcus aureus infections. When treated with the new drug, 10 of 10 mice survived for seven days after infection with a lethal dose of antibiotic-resistant bacteria. By contrast, 9 of 10 mice that received no drug died within two days of infection. Cresomycin also suppressed bacterial growth in mice infected with antibiotic-resistant Escherichia coli and Pseudomonas aeruginosa.
When tested in cultured human cells, cresomycin didn’t cause notable damage. The researchers are now working with a nonprofit biotechnology accelerator to move the drug closer to clinical trials.
“We don’t yet know whether cresomycin and drugs like it are safe and effective in humans. But our results show significantly improved inhibitory activity against a long list of pathogenic bacterial strains that kill more than a million people every year, compared with clinically approved antibiotics,” says Myers.
—by Sharon Reynolds
Related Links
- Designing a Safer Antifungal Drug
- Immune Boost May Protect Against Multiple Hospital-Acquired Infections
- Antibiotic Can Help Prevent Common Sexually Transmitted Infections
- Using Viruses to Treat Antibiotic-Resistant Bacterial Infections
- Searching for New Antibiotics in the Human Body
- A Targeted Antibiotic for Treating Lyme Disease
- Immune Boost Fights Antibiotic-Resistant Infections in Mice
- New Antibiotic for Gonorrhea Advances in Trials
- Retooling an Old Antibiotic
- Stamping Out Superbugs: A Clear and Present Danger
- Antimicrobial (Drug) Resistance
References
An antibiotic preorganized for ribosomal binding overcomes antimicrobial resistance. Wu KJY, Tresco BIC, Ramkissoon A, Aleksandrova EV, Syroegin EA, See DNY, Liow P, Dittemore GA, Yu M, Testolin G, Mitcheltree MJ, Liu RY, Svetlov MS, Polikanov YS, Myers AG. Science. 2024 Feb 16;383(6684):721-726. doi: 10.1126/science.adk8013. Epub 2024 Feb 15. PMID: 38359125.
Funding
NIH’s National Institute of Allergy and Infectious Diseases (NIAID) and National Institute of General Medical Sciences (NIGMS); National Science Foundation; Illinois State Startup Funds; Singapore Agency for Science, Technology and Research; Deutsche Forschungsgemeinschaft.


