Boosting brain's waste removal system could improve Alzheimer's outcomes
May 4, 2021
Boosting brain's waste removal system could improve Alzheimer's outcomes
At a Glance
- A study in mice suggests that antibody therapies targeting amyloid-beta protein may be more effective after enhancing the brain's waste drainage system.
- The findings point to a potential strategy to help slow the progression of Alzheimer's.
The lymphatic system is sometimes called the body's waste removal system. It's a vital part of the immune system that helps organs remove waste and protect from infection. Lymphatic vessels run alongside blood vessels to transport immune cells and cellular waste products. The lymph fluid is then filtered through glands called lymph nodes and returned to the bloodstream.
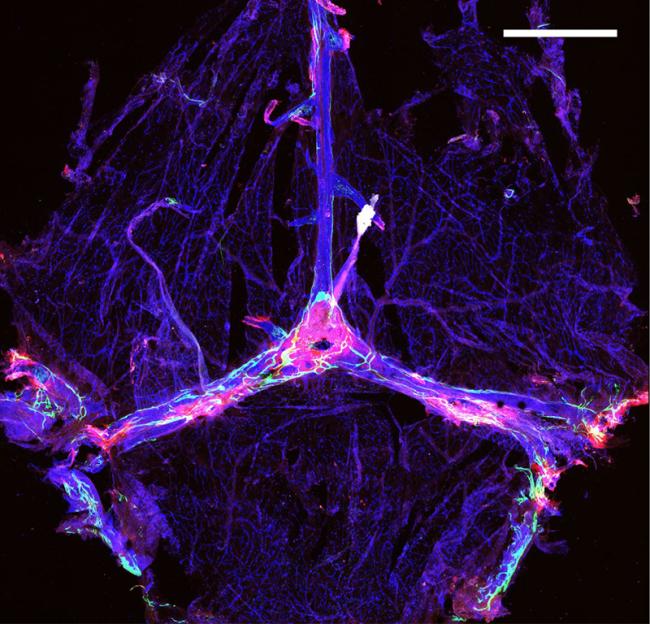
Just a few years ago, researchers discovered that the human brain has a lymphatic system of its own to remove waste. Recent studies suggest that problems with the brain's lymphatic clearance may play a role in Alzheimer's disease. One of the hallmarks of Alzheimer's is an abnormal buildup of amyloid-beta protein. A 2018 study found that impairing lymphatic vessels in a mouse model of Alzheimer's led to higher levels of amyloid-beta deposits in the brain as the mice aged.
A study led by Drs. Jonathan Kipnis, Oscar Harari, and Carlos Cruchaga of Washington University in St. Louis set out to investigate whether altering lymphatic drainage could make experimental antibody treatments that target amyloid-beta more effective. The study was funded in part by NIH's National Institute on Aging (NIA). Findings appeared in Nature on April 28, 2021.
Using a mouse model of early-onset Alzheimer's, the researchers removed some of the lymphatic vessels in the brains of one group of mice. They treated the mice, as well as a control group, with injections of antibody therapies, or "immunotherapies," including a mouse version of the drug aducanumab.
The mice with impaired lymphatic systems had greater buildup of amyloid-beta plaques and immune cells that cause inflammation. Brain inflammation is thought to play a role in Alzheimer's progression. These mice also performed more poorly on a test of learning and memory.
The researchers then tested whether boosting the brain's lymphatic system could have the opposite effect. They injected mice with a growth factor to enhance growth of cells that line the brain's lymph vessels. They then followed this with the amyloid-beta antibody therapies. The treated mice showed lower accumulations of amyloid-beta in the brain's meninges€”the membranes surrounding the brain and spinal cord.
A genetic analysis showed that microglia€”the brain's "trash collector cells"€”were greatly affected by manipulations of the brain's lymphatic system. When the team compared microglia in the brains of Alzheimer's patients with those of the mice whose lymphatic systems had been impaired, they found significant similarities.
Taken together, these findings support the role of impaired lymphatic drainage in the brain inflammation seen in Alzheimer's disease. The study also suggests that improving lymphatic clearance in people with Alzheimer's while administering immunotherapies could lead to better outcomes. Starting treatment early in the disease when the lymphatic system is more intact may be an important factor.
"A broad range of research on immunotherapies in development to treat Alzheimer's by targeting amyloid-beta has not to date demonstrated consistent results," says NIA Director Dr. Richard J. Hodes. "While this study's findings require further confirmation, the link it has identified between a well-functioning lymphatic system in the brain and the ability to reduce amyloid-beta accumulation may be a significant step forward in pursuing this class of therapeutics."
References
Meningeal lymphatics affect microglia responses and anti-Aβ immunotherapy. Da Mesquita S, Papadopoulos Z, Dykstra T, Brase L, Farias FG, Wall M, Jiang H, Kodira CD, de Lima KA, Herz J, Louveau A, Goldman DH, Salvador AF, Onengut-Gumuscu S, Farber E, Dabhi N, Kennedy T, Milam MG, Baker W, Smirnov I, Rich SS; Dominantly Inherited Alzheimer Network, Benitez BA, Karch CM, Perrin RJ, Farlow M, Chhatwal JP, Holtzman DM, Cruchaga C, Harari O, Kipnis J. Nature. 2021 Apr 28. doi: 10.1038/s41586-021-03489-0. Online ahead of print. PMID: 33911285.
Funding
NIH's National Institute on Aging (NIA); PureTech Health; Cure Alzheimer's Fund; Ed Owens Family Foundation; Archer Foundation.


