You are here
May 13, 2025
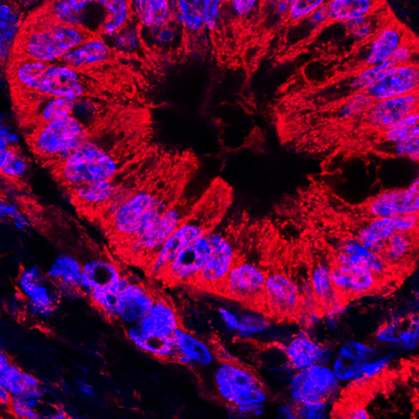
Disrupting fat metabolism may hinder pancreatic cancer
At a Glance
- Scientists were able to target a fat-recycling process to reduce pancreatic tumors in mouse and human models.
- The findings hint that interrupting fat-processing pathways could lead to new approaches for treating this often-deadly cancer.
Pancreatic cancer is one of the hardest types of cancer to treat. It rarely causes symptoms in its early stages. By the time symptoms arise, it’s usually at an advanced stage. Only about 13% of people diagnosed with pancreatic cancer are still alive five years later.
Previous studies have found that pancreatic cancer cells depend on the activity of lysosomes, which help to break down and recycle worn-out cell parts, for fuel. Some research suggests that blocking lysosomal processes might help to suppress the growth of pancreatic cancer. But to date, it’s been difficult for scientists to identify specific targets for drug development.
A research team led by Drs. Yuanyuan Qiao, Costas Lyssiotis, and Arul Chinnaiyan at the University of Michigan set out to identify metabolic vulnerabilities that could lead to potential treatments for pancreatic cancer. They studied the most common type of pancreatic cancer, called pancreatic ductal adenocarcinoma. The team zeroed in on an enzyme called PIKfyve, which is known to play a key role in the normal functioning of lysosomes. Results appeared in Nature on April 23, 2025.
The researchers first used genetically engineered mice to show that PIKfyve is not required for normal pancreatic development or function in healthy mice. However, it is essential to the development of pancreatic tumors. Mice lacking PIKfyve developed significantly less pancreatic cancer than mice with PIKfyve.
The scientists next asked whether experimental medications that block PIKfyve activity in the lab could block pancreatic tumor growth in mice. They tested two PIKfyve inhibitors, called ESK981 and apilmod, which have already cleared phase 1 clinical trials for other types of cancer. The compounds effectively blunted pancreatic tumor growth in mice.
The team studied human cell lines to learn what gene activity is affected by PIKfyve and its inhibitors. Many of the genes they found play a role in the metabolism of fatty acid molecules, or lipids. The activity was driven by the KRAS–MAPK signaling pathway, which is known to help control lipid metabolism. When PIKfyve is inhibited and the lysosomal recycling of lipids switches off, tumor cells can activate this pathway to generate their own fatty acid molecules for energy.
Additional experiments in the mouse and human models showed that disrupting both PIKfyve and the KRAS-MAPK pathway could reduce or eliminate pancreatic tumor cells. The findings suggest that simultaneously targeting these two pathways could be an effective approach for treating pancreatic cancer.
“Even though PIKfyve inhibitors have cleared phase 1 clinical trials for other cancers,” says lead author Caleb Cheng, “it was unclear how they worked to decrease tumor development and growth and whether they would work for pancreatic cancer.”
“The most exciting aspect of our findings is the discovery of a novel strategy to rewire lipid metabolism and significantly enhance the efficacy of KRAS inhibitors—therapies already approved for pancreatic cancer treatment,” Chinnaiyan adds.
—by Vicki Contie
Related Links
- Research in Context: Detecting Cancer
- Mapping How Cancers Form and Spread
- Keto Diet Enhances Experimental Cancer Therapy in Mice
- An mRNA Vaccine to Treat Pancreatic Cancer
- Identifying Potential Treatments for ALS
- Coronaviruses Hijack Lysosomes to Exit Cells
- Pancreatic Cancer
References: Targeting PIKfyve-driven lipid metabolism in pancreatic cancer. Cheng C, Hu J, Mannan R, He T, Bhattacharyya R, Magnuson B, Wisniewski JP, Peters S, Karim SA, MacLean DJ, Karabürk H, Zhang L, Rossiter NJ, Zheng Y, Xiao L, Li C, Awad D, Mahapatra S, Bao Y, Zhang Y, Cao X, Wang Z, Mehra R, Morlacchi P, Sahai V, Pasca di Magliano M, Shah YM, Weisman LS, Morton JP, Ding K, Qiao Y, Lyssiotis CA, Chinnaiyan AM. Nature. 2025 Apr 23. doi: 10.1038/s41586-025-08917-z. Online ahead of print. PMID: 40269157.
Funding: NIH’s National Cancer Institute (NCI), National Institute of Neurological Disorders and Stroke (NINDS), and National Institute of General Medical Sciences (NIGMS); U.S. Department of Defense; CRUK Scotland Centre; and Howard Hughes Medical Institute.
