Scientists design device for oral delivery of injections
October 29, 2019
Scientists design device for oral delivery of injections
At a Glance
- Scientists designed a capsule that, when taken by mouth, can deliver drugs through microneedle injections to the small intestine.
- After further development, the device could serve as an alternative to injections for drugs like insulin.
Biologic drugs are complex medications produced from living organisms or their parts. They include vaccines and drugs to treat conditions like rheumatoid arthritis, psoriasis, and cancer. Some biologic drugs, like insulin, can only be delivered by injection. If taken by mouth, stomach acid would destroy the drug before it could take effect.
Finding an alternative to injections would be ideal. Taking a medication orally causes less discomfort and does not result in used needles. Researchers have been working to develop ways to deliver biologic drugs orally.
A research team led by Drs. Robert Langer at the Massachusetts Institute of Technology (MIT) and Giovanni Traverso of MIT and Brigham and Women’s Hospital set out to design a system to deliver injectable drugs by mouth. The team worked in collaboration with scientists from the pharmaceutical company Novo Nordisk. Their study was funded in part by NIH’s National Institute of Biomedical Imaging and Bioengineering (NIBIB). Results were published in Nature Medicine on October 7, 2019.
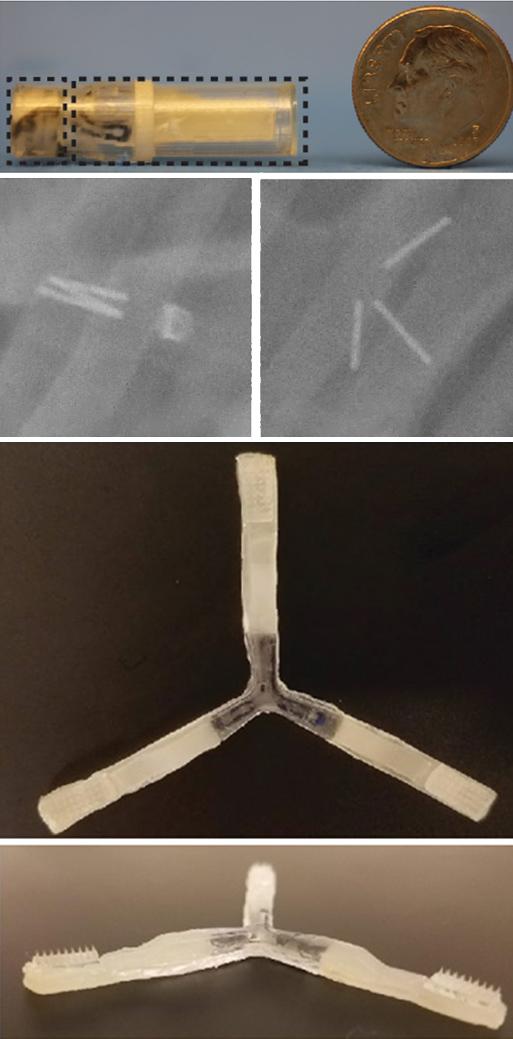
The team developed an ingestible capsule they named the “luminal unfolding microneedle injector” or LUMI. The device is roughly the size of a pen cap, measuring 9 mm (.35 inches) in diameter and 30 mm (1.2 inches) in length.
The capsule protects the LUMI during the acidic journey through the stomach and ejects the LUMI when it reaches the small intestine. Three spring-loaded arms extend, pushing a cluster of 1-mm long microneedles into the tissue wall of the small intestine. These microneedles dissolve, releasing the medication. The drug is then carried to the bloodstream.
The researchers developed their design based on tests using pigs and lengths of small intestine taken from humans. They worked to ensure that the microneedles penetrated the surface of the tissue without tearing through. Tests helped determine the ideal length of the device’s microneedles and the force with which the arms were deployed. The researchers note that the small intestine has few pain receptors. This ensures that the injections are not painful.
The team tested whether the LUMI device could effectively deliver insulin. Using pigs, the scientists compared needle injections to insulin administration via LUMI. They found that a significant amount of insulin could be delivered into the body with the device, and peak concentrations of insulin were reached more quickly compared to injection.
The team was able to confirm that the device broke into pieces after delivering the drug and was safely excreted from the body. This prevents blockages in the intestine.
The researchers note that the LUMI device has broad potential. “We can deliver insulin, but we see applications for many other therapeutics and possibly vaccines,” says Traverso. “We’re working very closely with our collaborators to identify the next steps and applications where we can have the greatest impact.”
—by Erin Bryant
Related Links
- “Intelligent” Injection Device Targets Tissues
- Protective Liquid Enables Oral Insulin Delivery in Rats
- Microneedle Patch Shrinks Fat Tissue in Mice
- Microneedle Patch for Flu Vaccine
- Injectable Nanoparticles Deliver Cancer Therapy in Mice
References
A luminal unfolding microneedle injector for oral delivery of macromolecules. Abramson A, Caffarel-Salvador E, Soares V, Minahan D, Tian RY, Lu X, Dellal D, Gao Y, Kim S, Wainer J, Collins J, Tamang S, Hayward A, Yoshitake T, Lee HC, Fujimoto J, Fels J, Frederiksen MR, Rahbek U, Roxhed N, Langer R, Traverso G. Nat Med. 2019 Oct 7. doi: 10.1038/s41591-019-0598-9. PMID: 3159160.
Funding
NIH’s National Institute of Biomedical Imaging and Bioengineering (NIBIB) and National Cancer Institute (NCI); Novo Nordisk; Massachusetts Institute of Technology; National Science Foundation; Bingham and Woman’s Hospital; Viking Olof Björk scholarship trust.


