SARS-CoV-2 may use key carbohydrate to infect cells
October 6, 2020
SARS-CoV-2 may use key carbohydrate to infect cells
At a Glance
- Researchers found that a carbohydrate called heparan sulfate, which is found on cell surfaces, may play a critical role in the novel coronavirus’ ability to infect cells.
- The findings suggest that the anti-clotting drug heparin may have potential to help combat coronavirus infections.
More than one million people have died worldwide from SARS-CoV-2 infection, the coronavirus that causes COVID-19. Researchers are racing to develop ways to treat and prevent new infections. Many of these treatments focus on blocking the virus’ ability to latch onto and infect cells in the body.
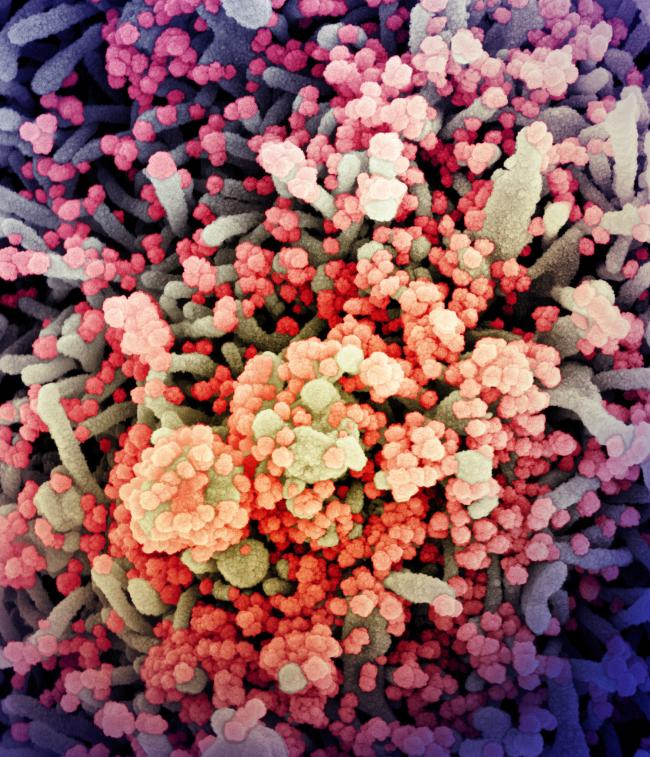
SARS-CoV-2 attaches to cells using its spike protein. This protein binds to the ACE2 receptor, a molecule that sits on the surface of human cells. After binding to ACE2, the virus undergoes a structural change that allows it to fuse with the cell. Once inside, the virus is able to reproduce.
To infect human cells, viruses must pass a dense layer of carbohydrates attached to the cell surface. This layer often includes the carbohydrate heparan sulfate. Several viruses, including herpes and other coronaviruses, are known to bind to heparan sulfate during infection. A team studying heparan sulfate, led by Drs. Thomas Clausen and Jeffrey Esko at UC San Diego, investigated whether the carbohydrate might also play a role in SARS-CoV-2 infection.
The study was funded in part by NIH’s National Heart, Lung, and Blood Institute (NHLBI), National Institute of Allergy and Infectious Diseases (NIAID), and National Institute of General Medical Sciences (NIGMS). Results were published in Cell on September 14, 2020.
The researchers found that both heparan sulfate and ACE2 are necessary for SARS-CoV-2 infection. Using molecular modeling, they identified where heparan sulfate binds the virus. They found that it interacts with a key part of the spike protein called the receptor binding domain (RBD).
They next used electron microscopy to examine how the drug heparin interacts with the RBD. Heparin is an FDA-approved medication similar in structure to heparan sulfate. It’s used to treat blood clots. The team found that when heparin or heparan sulfate attach to the RBD, they shift its structure to enhance its binding with ACE2. Further studies showed that SARS-CoV-2 must bind to both heparan sulfate and ACE2 to infect human lung cells grown in the lab.
The researchers were able to prevent infection by using enzymes to remove heparan sulfate from the cell surface. Heparin also blocked coronavirus infections in lab-grown cells by binding to the coronavirus and preventing it from entering cells.
The findings suggest that heparin could be repurposed to treat COVID-19. Blood clots and stroke are common complications from COVID-19, so many patients are already receiving the drug. The team estimates that the doses used to treat blood clotting would not completely prevent infection but might lead to a milder case.
“Our findings indicate that coronavirus infection requires heparan sulfate in addition to ACE2,” Esko says. “We imagine heparan sulfate may act as a ‘collector’ of the virus, enhancing the interaction between the spike protein and ACE2, and making viral infection more efficient.”
More studies are planned to explore whether heparin, heparan sulfate, or drugs that target heparan sulfate might translate into a COVID-19 treatment for people.
—by Erin Bryant
Related Links
- Computer-designed Proteins May Protect Against Coronavirus
- Immune Cells for Common Cold May Recognize SARS-CoV-2
- Potent Neutralizing Antibodies Target New Regions of Coronavirus Spike
- Experimental Coronavirus Vaccine is Safe and Produces Immune Response
- Potent Antibodies Found in People Recovered from COVID-19
- Unique Genomic Features of Fatal Coronaviruses
- Cancer Drug May Reduce Symptoms of Severe COVID-19
- Early Results Show Benefit of Remdesivir for COVID-19
- Llama Antibody Engineered to Block Coronavirus
- Microneedle Coronavirus Vaccine Triggers Immune Response in Mice
- Study Suggests New Coronavirus May Remain on Surfaces for Days
- Novel Coronavirus Structure Reveals Targets for Vaccines and Treatments
- Coronavirus Prevention Network
References
SARS-CoV-2 Infection Depends on Cellular Heparan Sulfate and ACE2. Clausen TM, Sandoval DR, Spliid CB, Pihl J, Perrett HR, Painter CD, Narayanan A, Majowicz SA, Kwong EM, McVicar RN, Thacker BE, Glass CA, Yang Z, Torres JL, Golden GJ, Bartels PL, Porell RN, Garretson AF, Laubach L, Feldman J, Yin X, Pu Y, Hauser BM, Caradonna TM, Kellman BP, Martino C, Gordts PLSM, Chanda SK, Schmidt AG, Godula K, Leibel SL, Jose J, Corbett KD, Ward AB, Carlin AF, Esko JD. Cell. 2020 Sep 14:S0092-8674(20)31230-7. doi: 10.1016/j.cell.2020.09.033. Online ahead of print. PMID: 32970989.
Funding
NIH’s National Heart, Lung, and Blood Institute (NHLBI), National Institute of Allergy and Infectious Diseases (NIAID), and National Institute of General Medical Sciences (NIGMS); National Science Foundation; Alfred Benzon Foundation; Massachusetts Consortium on Pathogen Readiness (MassCPR) grant; United States Department of Defense; Burroughs Wellcome Fund; Bill and Melinda Gates Foundation; Huck Institutes of the Life Sciences; Danish National Research Foundation; Innovation Fund Denmark; VAR2 Pharmaceuticals.


