SARS-CoV-2 can cause lasting damage to cells' energy production
August 22, 2023
SARS-CoV-2 can cause lasting damage to cells' energy production
At a Glance
- SARS-CoV-2, the virus that causes COVID-19, can cause lasting damage to energy production by mitochondria in many organs of the body.
- Stopping the virus from hijacking mitochondrial energy production may be a novel way to prevent serious complications from SARS-CoV-2 infection.
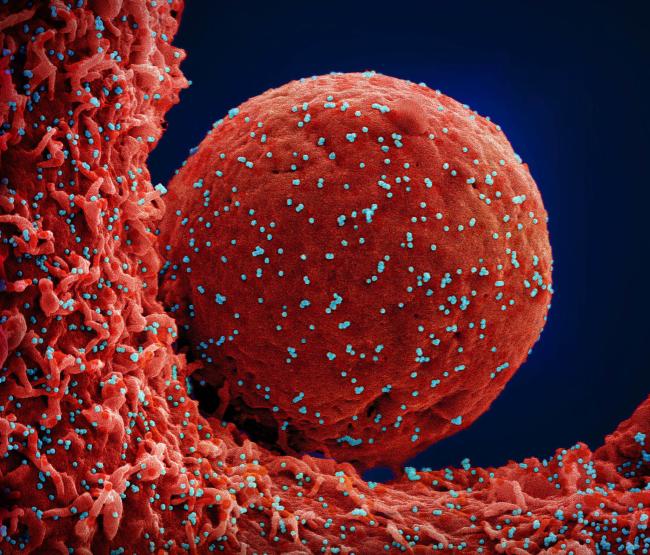
At the beginning of the COVID-19 pandemic, the virus responsible for the disease, SARS-CoV-2, was feared for its devastating damage to the lungs. But it quickly became apparent that the virus can infect organs and tissues throughout the body, including the heart, brain, kidneys, and blood vessels.
Much of the resulting dysfunction was thought to be the result of inflammation, the immune system's response to infection. But research has suggested that effects on mitochondria may also play a role in organ damage from SARS-CoV-2 infection. Mitochondria are the powerhouses of cells, producing most of the energy they need.
It's been known that parts of SARS-CoV-2 bind to proteins in the mitochondria. But how this affects mitochondrial function hasn't been clear. Dr. Afshin Beheshti, president of the nonprofit COVID-19 International Research Team and visiting researcher at Broad Institute, and Dr. Douglas Wallace from Children's Hospital of Philadelphia led an international team, including NIH researchers, to look more closely at the phenomenon.
The researchers compared mitochondrial gene expression€”when genes were activated€”in tissue samples taken from the nasopharynx of 216 people with COVID-19 and 519 uninfected people. They also looked at mitochondrial function in autopsy samples from the hearts, kidneys, livers, lungs, and lymph nodes of 35 people who died from COVID-19 compared with that from 5 people who died from other causes. The results were published on August 9, 2023, in Science Translational Medicine.
The team found that the expression of mitochondrial genes involved in energy production was suppressed in the nasopharynx during acute infection. This shifted cells into a state where they produced more of the substances the virus needs for replication. The researchers did not find this suppression in lung tissue samples taken after the virus had been cleared from the body.
Tissue samples taken during autopsies from the heart, kidney, liver, and lymph nodes continued to show suppression of these mitochondrial genes long after the virus had been cleared from the body. The reason for this continued suppression is unclear. In tandem with reduced mitochondrial function in these tissues, the researchers saw an upregulation of genes related to cellular stress.
"The continued dysfunction we observed in organs other than the lungs suggests that mitochondrial dysfunction could be causing long-term damage to the internal organs of these patients," Wallace says.
The team next used hamsters and mice to track mitochondrial function over the entire course of infection with SARS-CoV-2. They saw similar results in these animal models. Mitochondrial energy production was suppressed in the lungs during early SARS-CoV-2 infection, then bounced back once the immune system brought the virus under control. During early infection, mitochondrial gene expression was altered in the brain even though no SARS-CoV-2 was detected there, consistent with a systemic response to the virus.
The researchers also found a potential new target for treatment. They found that SARS-CoV-2 boosted expression of a regulatory molecule called miR-2392. This, in turn, lowered expression of mitochondrial genes involved in energy production.
"Neutralizing this microRNA might be able to impede the replication of the virus, providing an additional therapeutic option for patients who are at risk for more serious complications related to the disease," Beheshti says.
€”by Sharon Reynolds
References
Core mitochondrial genes are down-regulated during SARS-CoV-2 infection of rodent and human hosts. Guarnieri JW, Dybas JM, Fazelinia H, Kim MS, Frere J, Zhang Y, Soto Albrecht Y, Murdock DG, Angelin A, Singh LN, Weiss SL, Best SM, Lott MT, Zhang S, Cope H, Zaksas V, Saravia-Butler A, Meydan C, Foox J, Mozsary C, Bram Y, Kidane Y, Priebe W, Emmett MR, Meller R, Demharter S, Stentoft-Hansen V, Salvatore M, Galeano D, Enguita FJ, Grabham P, Trovao NS, Singh U, Haltom J, Heise MT, Moorman NJ, Baxter VK, Madden EA, Taft-Benz SA, Anderson EJ, Sanders WA, Dickmander RJ, Baylin SB, Wurtele ES, Moraes-Vieira PM, Taylor D, Mason CE, Schisler JC, Schwartz RE, Beheshti A, Wallace DC. Sci Transl Med. 2023 Aug 9;15(708):eabq1533. doi: 10.1126/scitranslmed.abq1533. Epub 2023 Aug 9. PMID: 37556555.
Funding
NIH's National Institute of Allergy and Infectious Diseases (NIAID); National Aeronautics and Space Administration; KBR Inc.; COVID-19 High-Performance Computing Consortium; Bill & Melinda Gates Foundation.


